In a groundbreaking study published in BMC Health Services Research, researchers led by Pokorny and colleagues have set their sights on the often-overlooked aspect of steady and effective follow-up care for patients undergoing grommet surgeries. These operations, integral to treating ear conditions such as otitis media, typically involve inserting small tubes into the eardrum to facilitate drainage and to prevent recurring infections. While the surgical procedure is widely recognized for its efficacy, the subsequent care practices post-surgery have not been thoroughly evaluated until now.
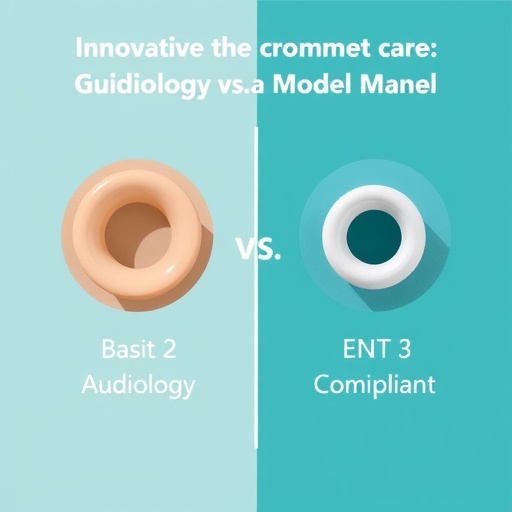
The study introduces a novel approach proposing audiology-led follow-up care, contrasting this model with the traditional ENT (Ear, Nose, and Throat) and nurse-led follow-up frameworks. The motivation behind this research arises from the critical need to optimize patient outcomes and streamline costs associated with post-operative care. The authors aim to challenge existing norms and suggest a new pathway that leverages the specialized skills held by audiologists.
In their meticulous comparison, the authors focus on key metrics that significantly impact both patient recovery experiences and healthcare expenditures. For instance, an audiology-led model may enhance access to care, as audiologists often provide services in various community settings, reducing the burden on specialized ENT facilities. This accessibility has the potential to lead to quicker response times for complications and more personalized care, addressing patients’ unique needs in a compassionate setting.
Research reveals that the success of medical interventions is heavily dependent on effective follow-up care. By establishing an audiology-led model, the study sheds light on the possibility of enhanced patient education regarding grommet care, allowing for greater patient engagement and empowerment in managing their health post-surgery. The researchers argue that such engagement may reduce the likelihood of complications and facilitate a deeper understanding of the surgical process and its implications.
The financial implications of this transition are equally compelling. The cost-effectiveness of the audiology-led model signifies not just savings for healthcare systems but also alleviates financial stress on families under the burden of medical expenses. Conducting a thorough cost comparison, the researchers found notable differences in overall expenditures associated with the three care models. Through strategic resource allocation and efficient use of clinician time, the audiology-led approach emerges as a frontrunner in promoting both fiscal responsibility and patient satisfaction.
Patient satisfaction surveys were administered, revealing that patients appreciated the structured counseling often provided by audiologists, which addressed common concerns and postoperative symptoms in a clear and reassuring manner. This aspect emphasizes how a shift in model can directly influence patient perceptions of care quality and health literacy. The study highlights how patients increasingly prefer care that is not only clinically effective but is also wrapped in a considerate, patient-centered approach.
One particularly compelling element of this research is the examination of outcomes related to hearing restoration following grommet placement. The study gathered data indicating that patient outcomes in terms of hearing improvements might also be optimized under an audiology-led model as these specialists are trained to monitor, assess, and provide interventions tailored to hearing health. This aspect could significantly enhance recovery trajectories for many children and adults alike.
As the healthcare landscape continues to evolve, multidisciplinary care models are becoming increasingly necessary. In the context of grommet follow-up, integrating audiologists into a more prominent role reflects a larger trend toward collaborative care approaches. This integrated style of care provides patients with a comprehensive support system, thereby improving the overall quality of healthcare delivery.
The implications of this research extend beyond just grommet follow-up; it reinforces the idea that specialist-led care can lead to improved outcomes across various disciplines within healthcare. As the authors highlight, the paradigm shift could serve as a model for reimagining how other postoperative care practices are administered, advocating for specialized expertise to take a more central role in patient care across the board.
The excitement surrounding this study also stems from its potential for shifting policy frameworks within healthcare systems. Regulatory bodies and healthcare administrators may find motivation to adopt the findings of this research into practice, reinforcing the idea that specialists like audiologists have critical roles in patient recovery and ongoing care.
Overall, the groundbreaking insight provided by Pokorny and colleagues presents a compelling case for change in the management of grommet follow-up care. The research not only offers a profound understanding of patient outcomes and costs but also inspires innovation and a rethinking of how we approach follow-up care in modern healthcare. It signals a future where specialized knowledge could strategically shape quality care models, ultimately benefiting patients and healthcare systems alike.
In sum, evolving healthcare delivery models necessitate continuous reflection on best practices. By establishing audiology-led follow-up care as a viable and desirable route, the authors provide an essential framework for future research and practice. This research is paving the way for a new standard, centered around patient needs and supported by sound clinical evidence.
The results from this investigation are poised to inspire healthcare providers and policy-makers to embrace and implement a more diverse array of follow-up care options, allowing an integrated model of care to emerge. Making audiologists central to grommet follow-up care could very well lead to improvements in both patient outcomes and system efficiencies, ultimately fostering a healthcare environment that prioritizes clinical excellence and compassionate care.
As we move forward, the implications of this study will resonate within the medical community. They present an opportunity to rethink how various specialties can collaborate to enhance the patient experience and the effectiveness of follow-up protocols. The findings of Pokorny et al. represent a promising roadmap for future advancements within otology and audiology, providing a crucial foundation for ongoing exploration and innovation.
The transformation in grommet follow-up care illuminated by this research will catalyze dynamic discussions across healthcare platforms, encouraging professional dialogue that could lead to broader changes in best practices. It stands as a vital contribution to the ongoing endeavor of ensuring that all patients receive comprehensive, informed, and responsive healthcare tailored specifically to their needs.
With a clear focus on the future of patient care, the implications of audiology-led follow-up care not only stand to benefit individuals with grommets but also offer a valuable template that can be applied across diverse healthcare contexts. As healthcare continues to evolve, this study represents a significant step toward more patient-centered, efficient, and effective health service delivery.
Subject of Research: Grommet follow-up care and the comparison of audiology-led, ENT-led, and nurse-led models.
Article Title: Reimagining grommet follow-up care: audiology-led outcomes and cost comparison with ENT (Ear, Nose and Throat) and nurse-led models.
Article References:
Pokorny, M.A., Snackers, MA., Phibbs, P. et al. Reimagining grommet follow-up care: audiology-led outcomes and cost comparison with ENT (Ear, Nose and Throat) and nurse-led models. BMC Health Serv Res 25, 1436 (2025). https://doi.org/10.1186/s12913-025-13610-y
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12913-025-13610-y
Keywords: audiology, grommet, follow-up care, patient outcomes, healthcare costs.
Tags: audiology-led patient carecommunity-based audiology servicesENT vs audiology model comparisongrommet surgery follow-up caregrommet surgery patient outcomeshealthcare cost reduction strategiesimproving access to ear careinnovative healthcare delivery modelsotitis media treatment effectivenesspatient recovery experience metricspost-operative care optimizationspecialized skills in audiology