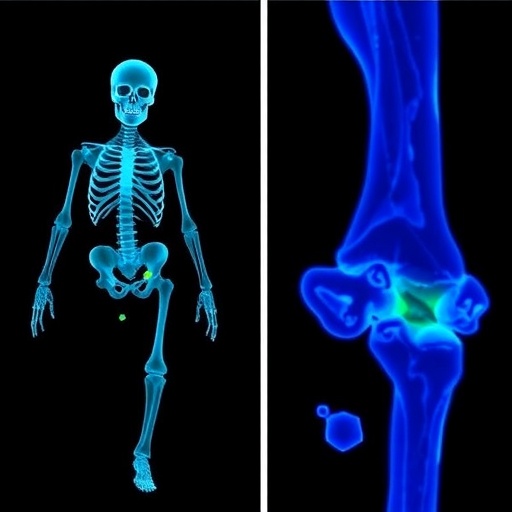
In a transformative leap for orthopedic medicine, researchers have developed a novel injectable hydrogel therapy that not only targets osteomyelitis but also reprograms cellular metabolism to fend off reinfection. Osteomyelitis, a challenging bone infection predominantly caused by bacteria such as Staphylococcus aureus, has long posed difficulties in treatment due to the intricate bone environment and persistent bacterial colonization. Traditional therapies often require prolonged systemic antibiotics and invasive surgeries, which carry significant risks and do not guarantee complete eradication. This pioneering approach, introduced in a recent publication in Nature Communications, promises a paradigm shift in managing chronic bone infections.
At the heart of this breakthrough is the design of a biocompatible hydrogel capable of being injected directly into infected bone sites, conforming to irregular bone cavities and delivering therapeutic agents with unparalleled precision. Unlike conventional antibiotic delivery systems that rely on systemic circulation and often fail to penetrate the bone microenvironment effectively, the hydrogel ensures sustained localized drug release. This approach minimizes systemic side effects and maximizes bacterial eradication within the niche environment where pathogens tend to hide.
More intriguingly, however, is the hydrogel’s ability to induce metabolic reprogramming of the infected tissue, a feature that distinguishes it from any existing treatment modality. Metabolic reprogramming refers to the profound alteration of cellular metabolism pathways, enabling cells to enhance their defensive capabilities against bacterial invasion. The hydrogel modulates the metabolic state of immune and bone cells, steering them towards phenotypes conducive to improved antimicrobial action and tissue repair. This metabolic shift results in a fortified microenvironment that not only eradicates the existing infection but also establishes resistance to future episodes.
The research team, led by Chen, H., Wei, L., and Yu, Q., engineered the hydrogel using a hybrid polymer matrix embedded with bioactive nanoparticles that release antimicrobial peptides and small molecules to recalibrate metabolic pathways. The hydrogel’s components were meticulously optimized to achieve a balance between mechanical strength, injectability, biodegradability, and bioactivity. The result is an injectable scaffold that seamlessly integrates into bone tissue, enhances local immune responses, and promotes osteogenesis.
In preclinical models of osteomyelitis, the hydrogel demonstrated remarkable efficacy. Animals treated with this novel system exhibited substantial reductions in bacterial load, rapid resolution of inflammation, and accelerated bone healing. Notably, when subjected to successive bacterial challenges, the treated bone sites showed significant resistance to reinfection, suggesting a durable protective effect conferred by the metabolic reprogramming. This finding is particularly compelling given the high rates of recurrence typically seen in osteomyelitis patients.
Diving deeper into the mechanistic insights, the study revealed that the hydrogel stimulates macrophages, pivotal immune cells in the bone, to adopt an M1-to-M2 polarization shift. The M1 phenotype is associated with pro-inflammatory and antimicrobial functions, whereas the M2 phenotype promotes tissue repair and resolution of inflammation. The hydrogel orchestrates a temporal sequence of activation that first aggressively targets bacteria and later nurtures tissue regeneration. Concurrently, osteoblasts, the bone-forming cells, experience metabolic remodeling that boosts their activity and resilience, counteracting the deleterious effects of infection and inflammation.
The intricate network of signaling pathways triggered by the hydrogel involves pivotal regulators such as AMP-activated protein kinase (AMPK) and hypoxia-inducible factor-1 alpha (HIF-1α), both central to cellular energy metabolism and response to stress. By modulating these pathways, the treatment enhances glycolysis and mitochondrial function, ensuring that immune and bone cells have the metabolic resources necessary to fulfill their protective and reparative roles. This metabolic fitness is crucial not only for clearing infection but also for establishing long-term tissue homeostasis.
Beyond its therapeutic implications, this hydrogel platform exemplifies an innovative strategy of leveraging cellular metabolism as a drug target in infectious diseases—a concept still in its infancy yet brimming with potential. Traditional antibiotics target bacterial structures and functions directly; however, targeting host metabolic pathways offers an orthogonal strategy that could circumvent antibiotic resistance, a mounting global health crisis. By empowering host cells metabolically, pathogens face an inhospitable environment that limits their survival and growth, effectively tipping the balance toward health.
The formulation process also emphasized minimizing adverse effects. The hydrogel components are derived from FDA-approved polymers and peptides known for their safety profiles, ensuring translational feasibility. Additionally, the hydrogel’s biodegradation timeframe is carefully balanced to prolong therapeutic function without hampering natural bone remodeling processes. This ensures patient safety and compatibility with standard clinical practices, paving the way for expedited clinical trials and eventual adoption in orthopedic wards.
Moreover, the delivery method—minimally invasive injection—offers significant advantages over current surgical debridement techniques. It reduces patient morbidity, shortens hospital stays, and lowers healthcare costs, making advanced osteomyelitis therapy accessible to a wider patient population globally. The adaptability of the hydrogel also allows for customization with various antimicrobial agents or immunomodulators, tailorable to specific bacterial strains or patient needs, thereby ushering in personalized bone infection treatment.
The interdisciplinary collaboration underlying this achievement cannot be overstated. The convergence of materials science, microbiology, immunology, and metabolic biology was critical in developing such a multifaceted therapeutic. The team’s success reflects the growing trend towards integrated biomedical research approaches that move beyond monotherapies to sophisticated bioengineering solutions addressing complex diseases holistically.
Looking forward, the researchers plan to explore the hydrogel’s application beyond osteomyelitis, considering other chronic infections and inflammatory bone disorders. There is also interest in combining the hydrogel with systemic immunotherapies and next-generation antibiotics to tackle multidrug-resistant bacterial strains that pose ever-increasing treatment challenges worldwide.
This cutting-edge research is not just a leap forward in osteomyelitis management but a beacon illuminating future directions in infection control. By harnessing the power of metabolic reprogramming via engineered biomaterials, medicine edges closer to developing smart, responsive therapies that adapt to the dynamic biological landscapes of chronic disease. Such innovations could transform intractable infections into manageable conditions, significantly improving patient outcomes and quality of life.
Ultimately, the injectable hydrogel platform represents a compelling fusion of technology and biology—transforming inert materials into active participants in healing processes. Its success highlights the tremendous potential of targeting host-pathogen interactions at the metabolic level, an approach poised to revolutionize not only orthopedics but infectious disease management as a whole. The medical world will undoubtedly watch closely as this promising technology progresses from laboratory discovery to clinical reality.
Subject of Research: Injectable hydrogels for the treatment of osteomyelitis and related metabolic reprogramming to prevent reinfection.
Article Title: Injectable hydrogels for osteomyelitis treatment induce metabolic reprogramming for protection against reinfection.
Article References: Chen, H., Wei, L., Yu, Q. et al. Injectable hydrogels for osteomyelitis treatment induce metabolic reprogramming for protection against reinfection. Nat Commun (2026). https://doi.org/10.1038/s41467-026-68318-2
Image Credits: AI Generated
Tags: advances in orthopedic treatmentsbiocompatible hydrogel therapychronic bone infection managementinjectable hydrogels for osteomyelitislocalized drug delivery systemsmetabolic reprogramming in infectionsminimizing systemic side effectsNature Communications publicationnovel treatment for osteomyelitisorthopedic medicine innovationsStaphylococcus aureus treatmenttargeted antimicrobial therapy