In an illuminating advancement that bridges the frontiers of neuroimmunology and regenerative medicine, recent research has unveiled a localized and inflammation-driven emergence of senescent-like glial cells within the complex pathology of multiple sclerosis (MS). This discovery not only reshapes our understanding of the cellular microenvironment in MS lesions but also underscores the potential of patient-derived organoids as transformative models for studying chronic neuroinflammatory diseases. The study, published in Nature Communications, reveals how glial senescence, triggered by spatially confined inflammatory cues, contributes to the relentless progression of MS, offering a compelling target for innovative therapeutic strategies.
Multiple sclerosis, a debilitating autoimmune disorder characterized predominantly by immune-mediated demyelination and neurodegeneration within the central nervous system (CNS), has long been studied through the prism of immune cell infiltration and axonal damage. However, the nuanced role of glial cells—specifically their senescent phenotypes—has remained elusive. Glia, encompassing astrocytes, microglia, and oligodendrocyte precursor cells, orchestrate CNS homeostasis and response to injury. Perturbations in their function and phenotype can critically influence disease trajectory. This investigation pioneers in delineating how localized inflammatory milieus induce a senescent-like state in glia, fundamentally altering their physiologic contributions and exacerbating neurodegenerative processes.
Senescence, classically associated with permanent cell cycle arrest and a distinct secretory profile termed the senescence-associated secretory phenotype (SASP), has predominantly been studied in the contexts of aging and cancer. Its emerging role within the CNS introduces a paradigm where senescent glial cells contribute to chronic inflammatory feedback loops and tissue dysfunction. By employing sophisticated spatial transcriptomics alongside immunohistochemical analyses, the researchers meticulously mapped senescence markers to discrete MS lesions. These spatially-resolved insights illuminate a patchwork of cellular states within the inflamed CNS, revealing senescent-like glia as pivotal players in lesion persistence and expansion.
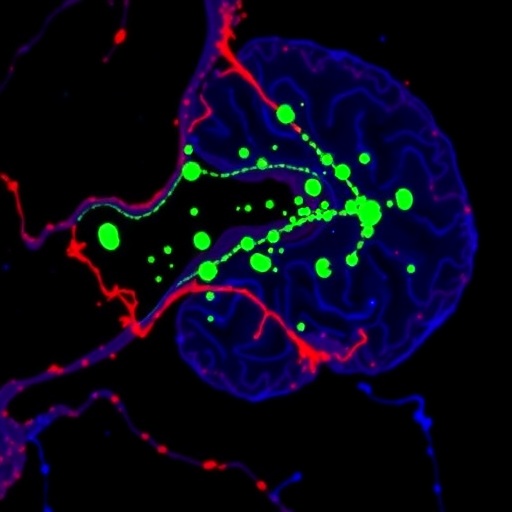
Crucially, the study leveraged patient-derived cerebral organoids as an ex vivo platform to recapitulate the inflammatory environment observed in MS. These three-dimensional, stem cell-derived mimetics faithfully encode donor-specific genetic and epigenetic landscapes, permitting robust investigation of disease-specific cellular dynamics. By exposing organoids to pro-inflammatory stimuli, the team faithfully elicited senescent-like phenotypes within glial populations, mirroring in situ observations. This methodological breakthrough establishes organoids not only as models for mechanistic inquiry but also as potential translational tools for therapeutic screening and personalized medicine.
Delving into the molecular signature of senescent-like glia uncovered upregulation of classical markers such as p16^INK4a^ and p21^CIP1/WAF1^, alongside a robust transcriptional signature enriched for cytokines, chemokines, and matrix remodeling enzymes. This SASP-like secretion pattern is hypothesized to propagate local inflammation, recruit peripheral immune cells, and impair remyelination. Such a chronic inflammatory niche likely tips the balance from resolution towards neurodegeneration, thereby driving progressive disability in MS patients. These findings challenge the conventional binary view of glia as merely reactive or supportive, positioning senescence as a critical node in pathological crosstalk.
The spatial restriction of senescent-like glia to lesion sites suggests that the inflammatory microenvironment intricately controls cellular fate decisions, revealing an interplay between immune signaling gradients and glial physiology. High-resolution imaging and cell lineage tracing within human tissue samples demonstrated that these senescent phenotypes are not uniformly distributed but instead clustered, typically at lesion borders or in proximity to immune infiltrates. Such distribution underscores the heterogeneity of CNS compartments in disease states and explains variable lesion activity observed clinically, often correlating with relapse frequency and severity.
Intriguingly, the research also examined the temporal emergence of glial senescence in relation to lesion development, suggesting a dynamic progression where initial glial activation transitions into senescence under sustained inflammatory stress. This chronification process may represent a tipping point whereby repair mechanisms falter, supporting a model wherein intermittent or chronic inflammation inexorably locks glia into pathological states. Understanding this timeline is pivotal, as it offers a window for therapeutic intervention before irreversible tissue damage ensues.
Therapeutic implications stemming from these findings are profound. Targeting senescent-like glia through senolytic or senomorphic agents—compounds designed to selectively eliminate or modulate senescent cells—could ameliorate neuroinflammation and promote lesion healing. The research emphasizes the need for CNS-penetrant drugs capable of modulating the senescence program without compromising essential cellular functions. Moreover, patient-derived organoids provide a promising platform to screen such therapeutics in a patient-specific manner, fostering the advent of precision neuroimmune therapies.
The methodology integrated cutting-edge technologies including spatial transcriptomics, single-cell RNA sequencing, and multiplexed immunofluorescence, reflecting the multidisciplinary approach required to dissect the intricate cellular ecosystems in MS. By correlating molecular signatures with pathological features across multiple patient samples, the study achieves both breadth and depth, ensuring that findings transcend individual variability and capture disease-generalizable mechanisms.
Moreover, the research signifies a broader shift in neurodegenerative disease conceptualization—from solely neuron-centered investigations toward appreciating the multifaceted roles of glial populations. Glial biology, long underappreciated, emerges as a fertile landscape for uncovering novel therapeutic targets. As glia are more numerous and versatile than neurons, interventions targeting these cells may substantially influence CNS health and recovery across a spectrum of disorders beyond MS.
This study further stimulates discourse on the concept of “inflammaging” within the CNS—where age-related inflammation and senescence intersect to exacerbate disease. Since MS often manifests in young adults but can accumulate progressive damage into later life stages, understanding how inflammation-induced senescence fits within this framework can enhance prognostic modeling and individual risk stratification. These insights could inform timing and nature of interventions, potentially delaying or preventing irreversible CNS deterioration.
The precision of patient-derived organoid models underscores their transformative potential in neuroscience research. These organoids encapsulate the complexity of human neurobiology while circumventing limitations of animal models that lack human-specific immune and inflammatory circuits. The ability to simulate pathological processes in a controlled yet physiologically relevant environment will undoubtedly accelerate drug discovery and mechanistic studies, catalyzing an era of personalized neuroimmunology.
Looking forward, integration of these findings with emerging bioinformatics and machine learning techniques could generate predictive models of lesion progression and response to therapy. Harnessing big data from spatially-resolved profiles and organoid assays will empower clinicians and researchers to devise tailored treatment regimens that preempt senescence-driven tissue damage, potentially altering disease course for the better.
Ultimately, this pivotal research encapsulates a paradigm shift that recognizes the dualistic nature of glial cells in MS—not only as responders to inflammation but as active contributors to disease chronicity via senescent transformations. By illuminating this intricate balance, the study opens novel investigative and therapeutic avenues that hold promise for millions affected by MS worldwide, heralding a new chapter in combating neuroimmunological disease.
Subject of Research:
Multiple sclerosis pathology focused on inflammation-induced senescent-like glial cells and modeling using patient-derived cerebral organoids.
Article Title:
Spatially-restricted inflammation-induced senescent-like glia in multiple sclerosis and patient-derived organoids.
Article References:
Fagiani, F., Pedrini, E., Martire, M.S. et al. Spatially-restricted inflammation-induced senescent-like glia in multiple sclerosis and patient-derived organoids. Nat Commun 16, 8477 (2025). https://doi.org/10.1038/s41467-025-63371-9
Image Credits: AI Generated
Tags: astrocytes and microglia rolescentral nervous system autoimmunitychronic neurodegeneration modelsglial cell senescence mechanismsimmune-mediated demyelinationinflammation-driven senescent glialocalized inflammatory cues in MSmultiple sclerosis pathologyneuroinflammatory diseases researchpatient-derived organoidsregenerative medicine advancementstherapeutic targets in MS