In a groundbreaking study published in the upcoming November 2025 issue of The American Journal of Emergency Medicine, researchers from Henry Ford Health and Michigan State University Health Sciences have illuminated a profound transformation in the utilization of hospice and palliative care (HPC) consultations initiated within emergency departments (EDs). The comprehensive analysis of over 8,000 HPC consults spanning seven years at five metropolitan Detroit emergency departments reveals a significant cultural and clinical shift that is reshaping the role of emergency medicine in end-of-life care. This research offers vital insights into how emergency care is evolving to better meet the complex needs of patients facing serious and terminal illnesses.
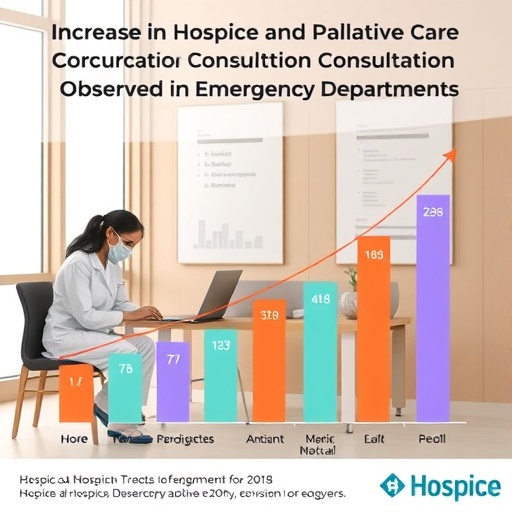
Historically perceived primarily as centers for acute interventions, emergency departments are increasingly serving as crucial initial points of contact for individuals requiring specialized palliative assessments and hospice referrals. The study meticulously tracks the trajectory of HPC consults from 2016 through 2023, underscoring a pronounced increase in palliative care consultations, which now constitute nearly 60% of all hospice and palliative care interactions in the ED. This pivot towards early palliative involvement marks a departure from traditional practices where such care was deferred until hospital admission or post-discharge community management.
The distinction between hospice and palliative care is essential to understanding the study’s implications. While hospice care is typically reserved for patients nearing the terminal phase of illness, with an emphasis on comfort rather than curative treatment, palliative care encompasses a broader spectrum, offering relief from symptoms and stress at any stage of a serious illness, irrespective of prognosis. The data reveal an intriguing inverse relationship between hospice referrals and palliative care consults over the analyzed period, with hospice referrals declining from nearly half to less than a quarter, concomitant with palliative care consults doubling to over half of all HPC engagements.
This evolution is particularly pronounced in the context of the COVID-19 pandemic. The surge in HPC consultations by 173.6% post-pandemic illustrates the heightened awareness and integration of palliative services within emergency medicine, triggered by the unprecedented challenges the pandemic posed to healthcare systems globally. The complexity and acuity of COVID-19 cases undoubtedly accelerated the recognition that emergency departments are pivotal arenas for initiating conversations about care goals, symptom management, and quality of life considerations among seriously ill patients.
Fabrice Mowbray, the study’s supervising author and director of the Data Center at Michigan State University College of Nursing, emphasizes that the pandemic underscored the indispensable role palliative care plays in the ED setting. This heightened recognition is reflective of a broader, systemic trend as hospitals across the nation increasingly embed palliative services within acute care frameworks. National data corroborate this shift, with the presence of palliative care teams in hospitals with over 50 beds surging from a mere 20% in 2000 to 84% by 2022. The integration of such teams is not merely an operational adjustment but represents a cultural shift toward proactive, patient-centered management of complex illnesses in emergent contexts.
The study’s findings further signal that early palliative interventions can foster improved outcomes—including enhanced goal-concordant care, increased patient and family satisfaction, and overall better quality of life during the often challenging terminal stages. This trend is supported by a growing body of literature advocating for the expansion of HPC access both within emergency and inpatient hospital settings. Such expansion enables tailored symptom relief and psychosocial support, which are essential to the holistic management of life-limiting diseases.
Satheesh Gunaga, the lead author and an emergency physician at Henry Ford Health, notes that while palliative care as a formally recognized specialty is relatively young—having only been board-certified in 2006—its rapid ascendance within emergency medicine circles reflects a growing commitment to addressing the needs of one of the most vulnerable patient populations. The emergency department, often the first point of contact during crises, offers a unique opportunity to promptly identify and address the complex care requirements that characterize serious illness trajectories, thereby preventing unnecessary hospitalizations and invasive procedures misaligned with patient goals.
The comprehensive nature of this study, which evaluated thousands of individual consults across multiple institutions, adds considerable weight to the evidence supporting integration of HPC in emergency medicine workflows. By scrutinizing utilization patterns and temporal trends, the researchers have provided critical benchmarks for healthcare providers and policy makers aiming to optimize the continuum of care for seriously ill patients. It is evident that emergency departments are no longer mere gateways to acute care but are evolving into pivotal interfaces where prognostic conversations, advance care planning, and symptom management begin.
Furthermore, the study highlights the essential need for ongoing education, policy formulation, and targeted research to support the sustained growth and efficacy of HPC programs in emergency settings. The rapidly increasing demand for these services necessitates well-coordinated interdisciplinary collaboration and resource allocation—challenges that institutions must address to scale HPC access without compromising quality or feasibility.
The notable shift from hospice to palliative care consults uncovered in this research may also reflect enhanced provider awareness of palliative care’s applicability beyond end-of-life scenarios, thus broadening the scope of immediate clinical interventions in the ED. This paradigm fosters a more nuanced understanding among emergency clinicians, allowing them to initiate early symptom control and psychosocial support that may delay or prevent hastened hospice enrollment, often perceived as signaling imminent death.
In addition to clinical impacts, the integration of HPC consults within emergency departments may ease the healthcare system’s burden by reducing futile or non-beneficial interventions. Efficient palliative care can align treatments with patient preferences, potentially reducing intensive care unit admissions and readmissions, which carry significant economic and emotional costs. These practices contribute to overall system sustainability while respecting patient dignity and autonomy.
Henry Ford Health and Michigan State University’s collaboration, exemplified in this research, embodies the transformative potential of academic-health partnerships. By combining clinical expertise, methodological rigor, and a commitment to community health, these institutions champion a future where emergency medicine and palliative care synergistically improve patient experiences and outcomes.
As the field advances, it becomes increasingly clear that the emergency department—once focused narrowly on acute, life-saving interventions—is now at the forefront of a revolution in compassionate, patient-centered care for those contending with serious illness. This evolution demands that healthcare providers not only refine clinical practices but also foster systemic transformations that prioritize early, integrated conversations about care preferences and quality of life.
Ultimately, this landmark study serves as a clarion call for the broader healthcare community to recognize and act upon the critical role that emergency department-initiated hospice and palliative care consultations play in shaping the future of care for seriously ill patients nationwide. The intersection of emergency medicine with palliative principles offers a promising avenue to ameliorate suffering, honor patient values, and enhance the humanity of healthcare during life’s most vulnerable moments.
Subject of Research: Hospice and palliative care consultations initiated in emergency departments.
Article Title: Trends in hospice and palliative care consults initiated in the emergency department: An eight-year utilization analysis.
News Publication Date: September 2025.
Web References:
Henry Ford Health + Michigan State University Health Sciences: http://henryfordmsu.org
MSUToday Article: https://msutoday.msu.edu/news/2025/09/emergency-departments-report-more-consults-for-hospice-palliative-care
Journal DOI: http://dx.doi.org/10.1016/j.ajem.2025.08.001
References:
Mowbray, F., Gunaga, S., et al. (2025). Trends in hospice and palliative care consults initiated in the emergency department: An eight-year utilization analysis. American Journal of Emergency Medicine. DOI: 10.1016/j.ajem.2025.08.001
Keywords: Health care, hospice care, palliative care, emergency medicine, end-of-life care, healthcare utilization, COVID-19 impact, patient-centered care, symptom management.
Tags: analysis of hospice consultationscultural shift in emergency medicineemergency department consultations for serious illnessesemergency department role in end-of-life careemergency medicine and hospice integrationevolving practices in emergency carehospice and palliative care consultationsincrease in palliative care referralsinterdisciplinary approach to end-of-life carelong-term palliative care trendspalliative care in urban healthcare settingspatients with terminal illnesses