In 2024, a remarkable 57.5 percent of the commercially insured population in the United States was found to have at least one chronic condition, according to an extensive report released by FAIR Health. This revelation adds urgency to ongoing public health discussions and underscores the tremendous healthcare burden carried by chronic diseases in America. Chronic conditions, which are often long-lasting and require continuous management, show a significant impact not only on patient well-being but also on healthcare costs nationwide.
The average allowed amount—essentially the maximum insurers cover for healthcare services—was nearly doubled for patients managing a single chronic condition compared to those without any. Patients with no chronic ailments had an average allowed amount of approximately $1,590, whereas those with one chronic condition faced nearly twice that cost, at approximately $3,039. These figures highlight the profound financial implications that accompany the diagnosis and treatment of chronic diseases.
Among the 44 chronic conditions examined, hyperlipidemia, commonly referred to as high cholesterol, was the most prevalent, with a crude prevalence of 21.2 percent within the commercially insured population. This condition, characterized by elevated levels of lipids in the blood, significantly contributes to the risk of cardiovascular diseases and is a critical target for intervention in efforts to reduce chronic disease burden.
The study further reveals that many patients suffer from multiple chronic conditions simultaneously, amplifying the complexity of care required and escalating healthcare expenditures. For instance, 11.5 percent of patients had two chronic conditions, while 9.1 percent bore the challenge of managing three. The coexistence of multiple conditions, termed comorbidities, significantly increases the demand for coordinated and comprehensive care strategies.
Notably, certain chronic conditions frequently appear together. Hyperlipidemia, hypertension, and obesity showed a substantial overlap, with 33.4 percent of patients having one or more of these conditions. Moreover, 4.3 percent of patients suffered from all three simultaneously, illustrating a concerning clustering of metabolic and cardiovascular risks that complicate treatment paths and health outcomes.
FAIR Health’s report emphasizes the correlation between the number of chronic conditions and healthcare spending. Costs rise incrementally with each additional condition, culminating in an average annual spending of $21,730 for patients with ten or more chronic conditions. This figure is a staggering 13.7 times higher than that for patients without any chronic conditions, highlighting the exponential escalation of healthcare resource needs as comorbidities accumulate.
Diving deeper, the study uncovers that different chronic conditions vary significantly in terms of their average cost and the number of co-occurring disorders. For example, lung cancer surfaced as the costliest condition, with an average annual allowed amount of $22,740, reflecting the intensive treatments and care required. On the other hand, attention deficit hyperactivity disorder (ADHD) was associated with the lowest average spending, at $4,175, demonstrating the spectrum of financial impact across chronic ailments.
The research also explored the median co-morbidity burden, identifying acute myocardial infarction, as well as Alzheimer’s and non-Alzheimer’s dementia, as conditions with the highest median number of additional chronic diseases—standing at six. By contrast, pneumonia and autism presented the least median co-morbidities, each associated with a median of just one other chronic condition, indicating distinct patterns in how chronic conditions associate with one another.
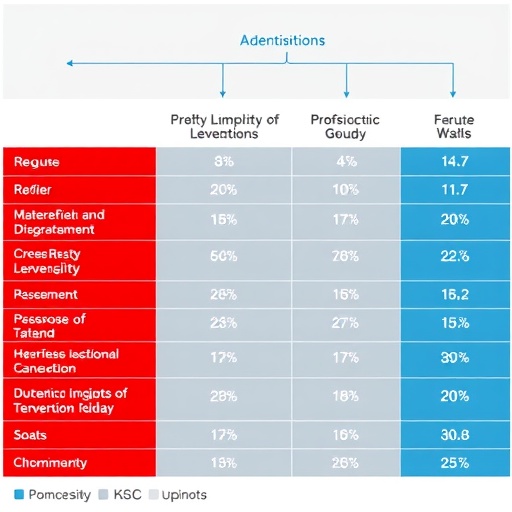
A notable aspect of the study lies in the statistical correlation between key chronic conditions prevalent in the American population. Hypertension, hyperlipidemia, obesity, and diabetes showed a range of positive correlations in their prevalence rates, with hypertension and diabetes demonstrating the strongest linkage at 86 percent. This strong association speaks to shared risk factors and overlapping pathophysiological mechanisms underpinning these diseases.
Adding a socioeconomic dimension, the research examined how chronic condition prevalence correlates with poverty at the county level. Clusters involving hypertension, diabetes, obesity, chronic kidney disease, and hyperlipidemia were all positively correlated with higher poverty rates, suggesting that economic disadvantage plays a critical role in the distribution and burden of these illnesses. Conversely, cancers encountered an inverse correlation with poverty, highlighted by breast cancer’s negative 24.3 percent correlation with poverty levels, possibly indicating differences in access to care, screening, and lifestyle factors.
The implications of these findings are profound, resonating across the healthcare ecosystem. Patients, clinicians, insurers, policymakers, and researchers all stand to benefit from a clearer understanding of the landscape of chronic diseases, their financial impacts, and their interrelationships. Such insights pave the way for more targeted interventions, improved resource allocation, and policies that address the social determinants of health influencing disease prevalence and outcomes.
FAIR Health’s forthcoming Epidemiological Reporting Platform, the FAIR Health Atlas, promises to further revolutionize the interpretation of chronic disease data. By leveraging the nation’s largest repository of commercial healthcare claims, this platform will enable dynamic mapping of disease prevalence, comorbidity patterns, and cost analyses across geographies and demographics. It will also facilitate exploration of the complex relationships between chronic conditions and social risk factors such as poverty.
At its core, the 2024 FAIR Health study underscores that chronic diseases represent a multifaceted challenge deeply intertwined with healthcare costs, patient quality of life, and social conditions. Efforts to mitigate the growing burden must combine clinical innovation, policy reform, and public health initiatives tailored to the realities of comorbidity and socioeconomic disparity.
The FAIR Health report is available in full detail and provides a comprehensive resource for stakeholders aiming to improve healthcare delivery and outcomes in the face of rising chronic condition prevalence. Its rich datasets and analyses serve as a foundation for ongoing research and strategies aimed at enhancing the lives of millions managing chronic diseases across the United States.
Subject of Research: Chronic Conditions Prevalence and Healthcare Costs in Commercially Insured U.S. Population
Article Title: Chronic Conditions in the United States: A Study of Commercial Claims
News Publication Date: February 2, 2026
Web References: https://s3.amazonaws.com/media2.fairhealth.org/whitepaper/asset/Chronic%20Conditions%20in%20the%20United%20States.pdf
Image Credits: Copyright 2026, FAIR Health, Inc. All rights reserved.
Keywords: Cholesterol, Chronic Conditions, Healthcare Costs, Comorbidity, Epidemiological Reporting, Hypertension, Diabetes, Obesity, Lung Cancer, Attention Deficit Hyperactivity Disorder, FAIR Health Atlas
Tags: average allowed amounts for chronic disease treatmentcardiovascular disease risk factorschronic conditions statistics 2024commercially insured population health trendsFAIR Health report findingsfinancial impact of chronic illnesseshealthcare burden of chronic conditionshealthcare costs for chronic diseasesmanaging chronic health conditionspatient well-being and chronic diseasesprevalence of hyperlipidemia in the USpublic health discussions on chronic illnesses