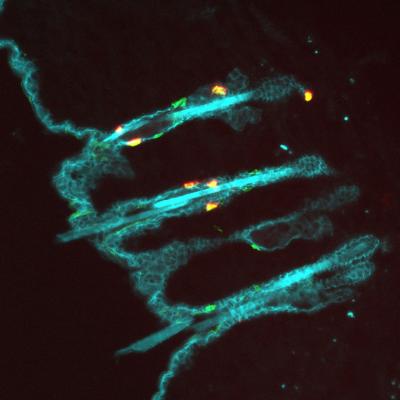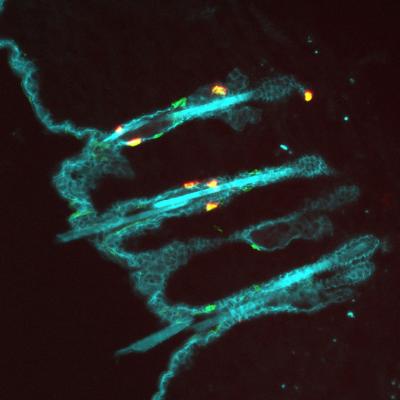
Credit: Yina Huang
In a newly published study, researchers at Dartmouth's Norris Cotton Cancer Center find that unique immune cells, called resident memory T cells, do an outstanding job of preventing melanoma. The work began with the question of why patients with melanoma who develop the autoimmune disease called vitiligo, have such a good prognosis. Vitiligo is an autoimmune skin condition against normal healthy melanocytes, which causes the loss of skin pigmentation in blotches. Using mouse models of melanoma and vitiligo, the research team found that resident memory T cells permanently reside in vitiligo-affected skin, where they kill melanoma cells. Although resident memory T cells were previously known to prevent skin viral infection, it was not known that they could fight tumors.
The research study, led by Mary Jo Turk, PhD, sought to understand why patients with metastatic melanoma who develop vitiligo during their course of treatment have been shown to survive longer. Using a mouse model of vitiligo, Turk addressed why this disease might be associated with a better clinical response. The study demonstrates for the first time that resident memory T cells are generated in response to a tumor, naturally as a result of autoimmune vitiligo, and serve a critical role in protecting against future tumors. Their study, "Resident memory T cells in the skin mediate durable immunity to melanoma" will be published in the next issue of Science Immunology.
This finding is surprising, because T cells that fight cancer have previously been thought to reside only in immune organs such as spleen, lymph nodes, and blood and enter tumors from the blood. "Our studies challenge this long-held belief by showing that tumor-killing T cells already reside in skin, where they can rapidly respond and kill melanoma cells" said Turk. Although these current studies are limited to mice, the presence of similar cells might explain why human patients with vitiligo are so well protected against melanoma and survive longer. Turk and her team plan to look for these cells in human patients.
"While we have shown that these T cells can kill melanoma in skin, we still need to determine whether they exist in other organs such as lung, where metastatic melanoma grows" said Turk. "Since our study identifies that resident memory T cells are critical for protection against tumors, and that T cells in skin provide long-term immunity to melanoma, the generation of such cells should be the goal of future cancer therapies."
###
Mary Jo Turk, PhD is an Associate Professor of Microbiology and Immunology at Dartmouth's Geisel School of Medicine. She serves as Co-Director of Norris Cotton Cancer Center's Immunology and Cancer Immunotherapy Research Program.
About Norris Cotton Cancer Center at Dartmouth-Hitchcock
Norris Cotton Cancer Center combines advanced cancer research at Dartmouth's Geisel School of Medicine with patient-centered cancer care provided at Dartmouth-Hitchcock Medical Center in Lebanon, NH, at Dartmouth-Hitchcock regional locations in Manchester, Nashua and Keene, NH, and St. Johnsbury, VT, and at partner hospitals throughout New Hampshire and Vermont. It is one of 45 centers nationwide to earn the National Cancer Institute's "Comprehensive Cancer Center" designation. Learn more about Norris Cotton Cancer Center research, programs, and clinical trials online at cancer.dartmouth.edu.
Media Contact
Lara Stahler
[email protected]
http://www.dhmc.org/webpage.cfm?org_id=796
############
Story Source: Materials provided by Scienmag