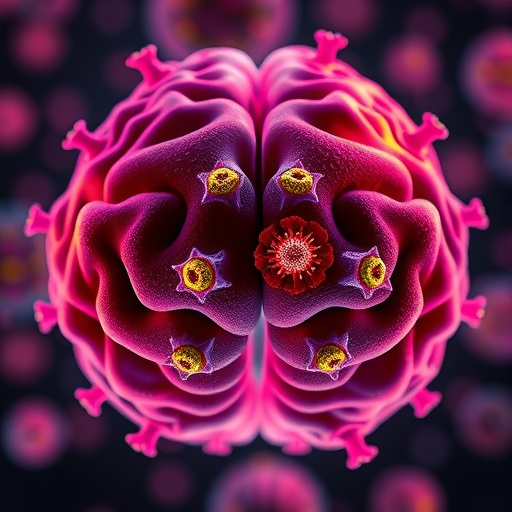
Mast Cells: The Brain’s Unsung Guardians Against Infection
For decades, mast cells have been primarily recognized as the immune system’s harbingers of allergic reactions, responsible for the itching, redness, and swelling millions endure each allergy season. These specialized cells respond rapidly to perceived threats by releasing histamine-laden granules, triggering inflammation and defense mechanisms. However, groundbreaking research from Washington University School of Medicine in St. Louis has unveiled a novel and critical function of mast cells beyond their role in allergies: protecting the brain from bacterial and viral invasion by regulating the delicate balance of cerebrospinal fluid (CSF) dynamics at the brain’s interface.
In an illuminating study recently published in the journal Cell, researchers explored how mast cells operate at microscopic “gates” embedded within the dura mater—the outermost protective membrane enveloping the brain. These tiny channels facilitate the clearance of metabolic waste from the brain’s interstitial space into lymphatic vessels, a pathway essential for maintaining neural homeostasis. While these gateways permit vital fluid exchange, they also harbor inherent risks as potential portals for pathogens to infiltrate the central nervous system.
.adsslot_o2lL6hTYAK{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_o2lL6hTYAK{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_o2lL6hTYAK{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
By studying mouse models infected with bacterial strains known to cause meningitis—such as Streptococcus agalactiae and Streptococcus pneumoniae—the investigators demonstrated that mast cells serve as vigilant sentinels, activating promptly upon detecting pathogens in the dura. Upon activation, mast cells degranulate, releasing histamine molecules that induce vasodilation of veins traversing these gates. This vascular expansion effectively occludes the fluid pathways, temporarily sealing off the conduits and preventing the passage of harmful bacteria into the brain parenchyma.
The significance of this mechanism was underscored by comparative analyses revealing that mice deficient in mast cells exhibited increased bacterial infiltration across the dura, culminating in more severe brain infections. Conversely, strategic enhancement of mast cell activity before bacterial exposure markedly diminished the bacterial load, affirming the protective capacity these cells confer. This discovery not only illuminates a heretofore unknown immunological barricade at the brain’s protective borders but also inaugurates new possibilities for therapeutic intervention against deadly neuroinfections.
Mast cells do not act in isolation; their activation precipitates a rapid and robust immune response by recruiting neutrophils—specialized phagocytic immune cells adept at engulfing and neutralizing invading microbes. This coordinated cellular interplay ensures that pathogens are detained and eliminated efficiently at the dural interface before they can compromise sensitive neural tissues. Such an orchestrated immune defense underscores the evolutionary ingenuity embedded within the brain’s microenvironment.
Extending their inquiry into viral neuropathogenesis, the research team partnered with experts studying neurotropic viruses, including the West Nile virus—a flavivirus transmitted via mosquito vectors with known neuroinvasive properties. The findings revealed a parallel protective effect of mast cells against viral invasion. Mice lacking mast cells allowed higher concentrations of the West Nile virus to penetrate the brain, whereas those with intact mast cell function exhibited significantly reduced viral loads, indicating mast cells’ pivotal involvement in mounting antiviral defenses.
While the newfound role of mast cells in brain protection heralds promising strategies to bolster neuroimmune defenses, the researchers caution that prolonged or chronic mast cell activation may bear detrimental consequences. Sustained occlusion of CSF flow pathways could lead to the accumulation of metabolic “waste” products such as amyloid beta, a peptide notoriously associated with the pathogenesis of Alzheimer’s disease. This dualistic nature of mast cells emphasizes the necessity for precision in modulating their activity to leverage protective benefits while minimizing potential adverse outcomes.
Looking ahead, the investigative team aspires to dissect the fine line between beneficial acute mast cell responses and detrimental chronic activation states, with the ultimate aim of tailoring interventions that can vaccinate or precondition the brain’s immune gatekeepers. Such interventions could revolutionize approaches to combating bacterial meningitis, viral encephalitis, and potentially even neurodegenerative conditions characterized by aberrant waste accumulation.
This pioneering work opens an exhilarating chapter in neuroimmunology, recasting mast cells from mere instigators of allergic misery to indispensable guardians stationed at the neural frontier. Their ability to enact dynamic structural and cellular changes at the brain’s dura mater interface underscores a sophisticated, previously underappreciated layer of defense that bolsters the brain’s sanctity against microbial threats.
The interdisciplinary nature of the study—uniting immunologists, neurobiologists, infectious disease experts, and vascular physiologists—highlights the complexity and integrative nature of brain health. Unraveling the molecular signaling cascades that dictate mast cell activation and the subsequent vascular remodeling promises to yield novel molecular targets for drugs designed to fine-tune this defense system.
Moreover, the elucidation of these mechanisms in animal models paves the way for translational research aimed at validating whether similar pathways operate in humans. The implications are vast, potentially informing clinical practice in neurology and infectious disease management, and guiding the development of prophylactic therapies that enhance mast cell functions without tipping the balance toward pathological inflammation.
As the brain’s gatekeepers reveal their crucial functions, one thing is clear: mast cells occupy a central and dynamic role far beyond allergy-induced inflammation. Their newfound identity as protectors of cerebrospinal fluid flow and inhibitors of pathogen ingress challenges researchers to rethink long-held dogmas and inspires innovative avenues to safeguard brain health in the face of ever-present microbial threats.
Subject of Research: Animals
Article Title: Mast cells regulate the brain-dura interface and CSF dynamics
News Publication Date: 24-Jul-2025
Web References:
https://www.cell.com/cell/fulltext/S0092-8674(25)00748-2
References:
Mamuladze T, Zaninelli TH, Smyth LCD, Wu Y, Abramishvili D, Silva R, Imbiakha B, Verhaege D, Du S, Papadopoulos Z, Gu X, Lee D, Storck S, Perrin RJ, Smirnov I, Dong X, Song Hu, Diamond MS, Pinho-Ribeiro FA, Kipnis J. Mast cells regulate the brain-dura interface and CSF dynamics. Cell. July 24, 2025. DOI: 10.1016/j.cell.2025.06.046
Image Credits: Sara Moser
Keywords: Mast cells, Bacteria, Brain tissue, Meningitis, Immune cells
Tags: allergic reactions immune responsebrain infection defense mechanismscentral nervous system pathogenscerebrospinal fluid dynamicsdura mater protective membraneimmune guardians against pathogenslymphatic vessels brain clearancemast cells immune system brain protectionmeningitis bacterial infection studymicroscopic gates in brainneural homeostasis and infectionWashington University School of Medicine research