Hyperuricemia: A Comprehensive Overview of Current Understanding and Management Approaches
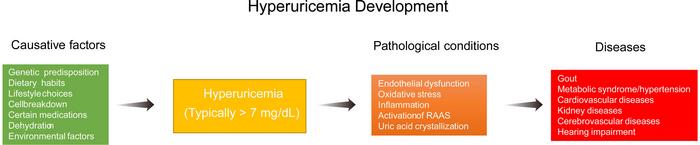
Hyperuricemia (HU) has emerged as a significant global health issue, manifesting as elevated uric acid (UA) levels in the bloodstream. This condition is primarily identified when UA concentrations exceed 420 µmol/L (7 mg/dL) in males and 350 µmol/L (6 mg/dL) in females. Underlying this seemingly straightforward threshold is a complex interplay of genetic, dietary, and environmental factors that influence uric acid metabolism. Unlike many other mammals that possess uricase, an enzyme responsible for converting UA into a more soluble compound, humans lack this capability, making them particularly susceptible to hyperuricemia and its associated health risks.
The ramifications of HU are alarming, particularly due to its close association with various chronic diseases, notably cardiovascular diseases (CVDs), gout, and metabolic syndrome. Elevated UA levels have been linked to endothelial dysfunction and increased oxidative stress, conditions that are intricately connected to the development of atherosclerosis. Furthermore, studies have shown that soluble UA may activate pathways of inflammation, exacerbating vascular injury and leading to adverse cardiovascular outcomes. The growing recognition of HU as a pivotal risk factor for gout reinforces its significance, as this inflammatory arthritic condition arises due to the deposition of urate crystals in joints, causing acute episodes of severe pain.
Moreover, hyperuricemia is increasingly recognized for its role in metabolic syndrome (MS). Approximately one-third of individuals diagnosed with MS exhibit elevated UA levels, further complicating management strategies for this multifaceted syndrome that correlates strongly with obesity, hypertension, and insulin resistance. The links between HU and renal function are equally concerning; persistently high UA levels can contribute to chronic kidney disease and acute kidney injury by impairing the kidneys’ ability to excrete uric acid effectively. A key focus remains on understanding how these associations can inform targeted interventions.
Diagnostic approaches to hyperuricemia are vital in establishing effective management plans. Traditionally, measuring serum uric acid levels has been the gold standard for diagnosing HU. However, the distinction between hyperuricemia and gout can prove challenging due to variations in metabolic profiles. Technological advancements have paved the way for enhanced diagnostic precision, utilizing non-invasive imaging techniques like ultrasound and dual-energy computed tomography to visualize urate crystal deposits in joints and tissues. These innovations are complemented by omics technologies, such as metabolomics and genomics, that identify biomarkers associated with hyperuricemia, contributing to more refined risk assessments.
As treatment guidelines for hyperuricemia evolve, pharmacological interventions remain central to management. The primary goal of pharmacotherapy is to lower uric acid levels effectively. Xanthine oxidase (XO) inhibitors, predominantly allopurinol and febuxostat, are recognized as first-line treatments. For patients struggling with treatment resistance, a combination of various pharmacological agents may be necessary. Emerging therapies, including lesinurad and interleukin-1 inhibitors, provide additional avenues for patients facing refractory hyperuricemia. Nonetheless, these pharmacological options are not without their challenges; the potential for adverse effects can lead patients toward alternative therapies.
Lifestyle factors, encompassing dietary habits and physical activity, are critical in shaping uric acid levels and overall health outcomes. Excessive intake of purine-rich foods, alcohol, and fructose, in conjunction with sedentary lifestyles, can markedly increase the risk of developing hyperuricemia. On the flip side, dietary interventions emphasizing plant-based foods can help promote uric acid excretion through urine alkalization. Engaging in regular physical activity offers additional benefits by enhancing insulin sensitivity and facilitating clearance of uric acid, although individuals should avoid excessive high-intensity exercise that may paradoxically elevate UA levels due to lactate production.
In light of the complexities surrounding hyperuricemia, future research must prioritize integrating insights from genetic studies that have illuminated polymorphisms in UA transporters and metabolic enzymes. These discoveries create pathways toward developing tailored treatment strategies that account for individual genetic makeups. Additionally, therapies targeting the human microbiome, including probiotics and fecal microbiota transplantation, hold promise for lessening the metabolic burden of hyperuricemia.
Despite advancements in our understanding of hyperuricemia, significant challenges remain. Optimizing the duration of treatments, determining the long-term efficacy of emerging therapies, and refining diagnostic criteria are key areas that warrant ongoing research. Collaborative efforts among clinicians, scientists, and policymakers will be essential in optimizing strategies for managing hyperuricemia effectively, ultimately improving patient health outcomes and quality of life.
In conclusion, hyperuricemia is a complex metabolic disorder with multifactorial origins and significant health implications. Emphasizing a comprehensive approach that considers genetic predispositions, environmental influences, and lifestyle factors is paramount in managing this condition. As research continues to uncover the intricacies of UA metabolism, including the potential roles of microbiota and alternative therapies, there is hopeful promise for enhancing treatment strategies that go beyond conventional pharmacological options. By promoting collaborative research efforts and integrating new scientific discoveries into clinical practice, we can forge a path toward improved health outcomes for individuals grappling with hyperuricemia and related conditions.
Subject of Research: Hyperuricemia
Article Title: Hyperuricemia: Current State and Prospects
News Publication Date: 2-Jan-2025
Web References: Exploratory Research and Hypothesis in Medicine
References: None Provided
Image Credits: Weizheng Zhang
Keywords: Hyperuricemia, Uric Acid, Cardiovascular Diseases, Gout, Metabolic Syndrome, Gut Microbiota, Treatment Strategies, Lifestyle Interventions
Tags: dietary impacts on hyperuricemiaelevated uric acid levels health risksendothelial dysfunction and uric acidenvironmental influences on uric acid levelsfuture research directions in hyperuricemiagenetic factors influencing uric acid metabolismgout as a consequence of hyperuricemiahyperuricemia management strategiesinflammation pathways in hyperuricemiametabolic syndrome and elevated uric acidoxidative stress and cardiovascular outcomesrelationship between hyperuricemia and cardiovascular diseases