Obesity’s role as a dominant risk factor for cardiovascular disease is well-established, yet the detailed mechanisms linking excess adiposity to changes in cardiovascular dynamics remain incompletely understood. Emerging research now shines a light on how the body’s central hemodynamics—the blood flow and pressures within the organs and large vessels close to the heart—adjust in response to increasing body mass. In a groundbreaking study published in the International Journal of Obesity, researchers reveal a complex relationship between body mass index (BMI) and key cardiovascular parameters, challenging earlier assumptions and highlighting hyperdynamic circulation as a potential hallmark of obesity.
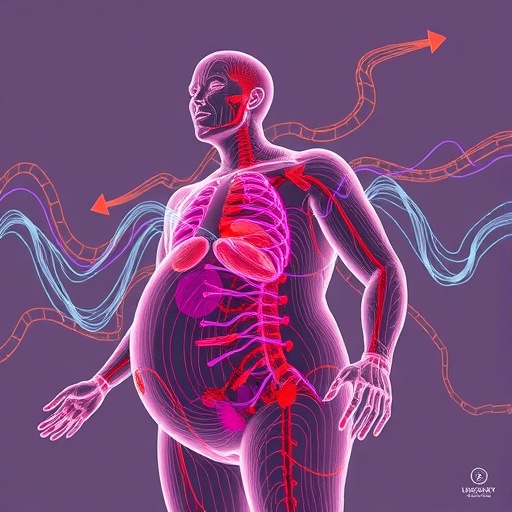
The study focused on two critical metrics: cardiac index (CI), which measures the heart’s output relative to body surface area, and systemic vascular resistance (SVR), the resistance the heart must overcome to pump blood through the systemic circulation. Traditionally, obesity’s cardiovascular effects have been attributed to elevated blood pressure and arterial stiffness; however, this research provides robust evidence that higher BMI correlates with a distinctive circulatory pattern characterized by increased CI and decreased SVR. This suggests that the hearts of individuals with higher BMI are in a perpetually hyperdynamic state, pumping more vigorously but encountering less vascular resistance, an intriguing adaptation or maladaptation with significant clinical implications.
Utilizing data from a large cohort of adult patients admitted for various medical reasons, the researchers conducted an extensive analysis comparing hemodynamic measurements across diverse BMI categories. The scale of the study distinguishes it from previous smaller, population-specific investigations, allowing for more generalizable conclusions. The findings underscore a consistent pattern: as BMI increases, the heart compensates by augmenting output, while peripheral blood vessels dilate or reduce resistance, possibly as a mechanism to maintain adequate tissue perfusion despite the metabolic demands of increased body mass.
This hyperdynamic circulation observed forms the physiological basis for many of the clinical manifestations seen in obesity. The elevated cardiac index indicates increased cardiac workload, potentially accelerating the progression to heart failure if sustained over long periods. Meanwhile, the reduction in systemic vascular resistance may initially serve as a protective mechanism, preventing excessive hypertension. Nevertheless, this adaptive response might have limits, and prolonged exposure to such altered hemodynamics could contribute to vascular remodeling, endothelial dysfunction, and eventual cardiovascular compromise.
Beyond establishing the associations, the study delves into potential mechanisms driving these changes. It is hypothesized that adipose tissue, once considered inert, actively secretes a plethora of bioactive substances—adipokines—that influence vascular tone and cardiac function. Additionally, the augmented metabolic demand in obese individuals may necessitate increased tissue perfusion, prompting the cardiovascular system to maintain elevated cardiac output. These insights open avenues for targeted therapeutic interventions aiming to modulate these hemodynamic parameters and mitigate cardiovascular risk.
The implications of this research extend to clinical practice, where a deeper understanding of obesity-induced hemodynamic alterations can refine risk stratification and management. Current cardiovascular assessments in obese patients might benefit from incorporating measurements of cardiac index and systemic vascular resistance to better gauge disease progression and response to treatment. Moreover, this evidence supports a more nuanced approach to managing hypertension in obesity, recognizing that blood pressure elevation in this population may stem from a fundamentally different hemodynamic profile than previously assumed.
Notably, the study’s approach circumvents the limitations of prior research by including a heterogeneous patient population and employing rigorous methods to account for confounding factors such as age, gender, and comorbidities. This robustness enhances confidence in the generalizability of the findings and positions hyperdynamic circulation as a unifying feature rather than an anomaly seen in isolated groups. Furthermore, longitudinal follow-ups could elucidate how these hemodynamic patterns evolve over time and their prognostic significance.
An intriguing aspect of hyperdynamic circulation is its duality—it reflects both a physiological adaptation to increased metabolic demands and a potential pathophysiological process leading to cardiovascular deterioration. The challenge lies in discerning when this state shifts from beneficial compensation to maladaptive consequence. Investigating biomarkers or imaging modalities sensitive to these transitions could revolutionize obesity-related cardiovascular care, enabling pre-emptive interventions before irreversible damage ensues.
The research also raises questions about the reversibility of these hemodynamic changes with weight loss or pharmacological modulation. If the hyperdynamic state is reversible, interventions such as bariatric surgery, lifestyle modification, or drugs targeting vascular resistance might restore more normal circulatory dynamics, reducing cardiovascular morbidity and mortality. Ongoing and future studies will be crucial in determining the effectiveness of such strategies and establishing clinical guidelines.
Moreover, understanding the interplay between obesity and hemodynamics may provide insights into other conditions characterized by altered vascular resistance and cardiac output, such as metabolic syndrome, diabetes mellitus, and even certain forms of heart failure. The findings encourage a holistic view of cardiovascular health that integrates metabolic status with hemodynamic function, fostering interdisciplinary collaboration between endocrinologists, cardiologists, and vascular specialists.
From a public health perspective, this research emphasizes the urgency of addressing obesity not merely as a matter of weight but as a complex condition with profound cardiovascular ramifications. The identification of hyperdynamic circulation as a hallmark encourages early screening and monitoring, potentially averting long-term complications. This paradigm shift reinforces the need for comprehensive obesity management programs that incorporate cardiovascular evaluation as an integral component.
Technological advancements in non-invasive hemodynamic monitoring played a pivotal role in enabling such large-scale, detailed analyses. Continuous improvement in these diagnostic tools will facilitate broader application in clinical settings, enabling real-time assessment and personalized care. Integrating artificial intelligence and machine learning may further enhance the interpretation and predictive power of hemodynamic data submitted by obese patients.
In conclusion, the novel insights provided by this study redefine our understanding of obesity and its cardiovascular consequences. The confirmation that hyperdynamic circulation typifies the obese state challenges clinicians and researchers to rethink diagnostic and therapeutic approaches. By recognizing elevated cardiac index and reduced systemic vascular resistance as central features, future efforts can focus on unraveling the underlying molecular pathways and developing targeted therapies, paving the way for improved outcomes in this growing patient population.
This research ultimately underscores the dynamic interplay between body mass and cardiovascular physiology, highlighting the body’s complex adaptations to excess adiposity. While obesity’s burden on health remains daunting, elucidating these fundamental mechanisms equips the medical community with knowledge to devise innovative strategies, bringing hope for more effective prevention and treatment of obesity-related cardiovascular disease.
As this field evolves, continuous investigation into the temporal nature of hyperdynamic circulation and its interaction with other comorbidities will be essential. Collaborative networks pooling data internationally may yield finer resolution insights and validate findings across ethnically and geographically diverse populations, thereby advancing global health equity in obesity care.
In an era where obesity prevalence reaches epidemic proportions worldwide, insights into hemodynamic adaptations serve as critical tools for mitigating cardiovascular risk. This study is a prime example of how meticulous investigation into physiological nuances can drive transformative change in understanding and managing multifaceted diseases, charting a promising course towards healthier futures.
Subject of Research: Central hemodynamics and their association with body mass index in obesity.
Article Title: Is hyperdynamic circulation a hallmark of obesity?
Article References:
Malm, E.H.J., Warrad, W., Hadad, R. et al. Is hyperdynamic circulation a hallmark of obesity?. Int J Obes (2025). https://doi.org/10.1038/s41366-025-01981-5
Image Credits: AI Generated
DOI: 12 December 2025
Tags: arterial stiffness and obesitybody mass index and cardiovascular healthcardiac index and systemic vascular resistancecardiovascular adaptations in obesitycardiovascular disease risk factorscomplex relationship between BMI and heart healthelevated blood pressure in obese individualshyperdynamic circulation in obesityInternational Journal of Obesity research findingsmechanisms linking obesity to cardiovascular dynamicsobesity and hemodynamicsobesity’s impact on heart function