When a virus makes its way into a person’s body, one of the immune system’s first responders is a set of pathogen-removal cells called macrophages. But macrophages are diverse; they don’t all target viruses in the same way.
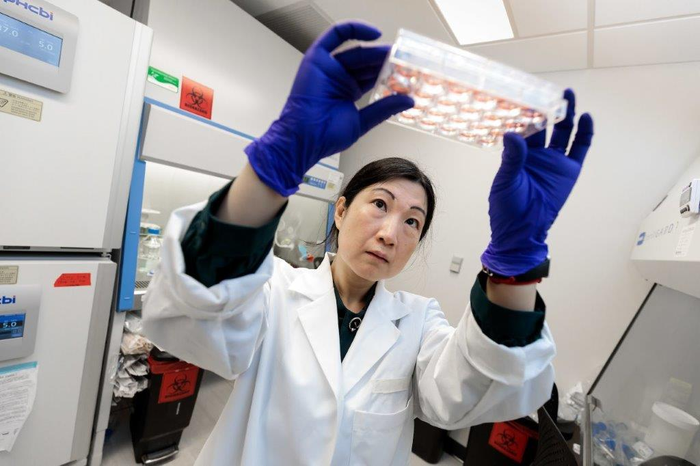
Credit: John Zich
When a virus makes its way into a person’s body, one of the immune system’s first responders is a set of pathogen-removal cells called macrophages. But macrophages are diverse; they don’t all target viruses in the same way.
Researchers at the University of Chicago’s Pritzker School of Molecular Engineering (PME) have discovered that the type of macrophages present in a person’s body might determine how likely they are to develop severe inflammation in response to COVID-19. Their study has been published in Nature Communications.
“Clinicians know that COVID-19 can cause a spectrum of disease severity from mild to severe symptoms. Why some people, and not others, develop very severe disease has been a mystery,” said Asst. Prof. Huanhuan Joyce Chen, who led the research with Qizhou Lian of the University of Hong Kong. “This is the first time anyone has linked the variation in symptoms to macrophages.”
A better model for COVID-19 infection
Studying the cellular and molecular effects of the SARS-CoV-2 virus has been challenging for researchers who usually turn to model organisms to mimic human diseases; mice, rats, and many other animals don’t develop the same COVID-19 symptoms as people. That’s why, shortly after the COVID-19 pandemic began, Chen’s group harnessed human stem cells to study the virus.
As reported previously in Nature, Chen and her colleagues grew stem cells into functioning mini-lungs and colons—called lung and colon organoids—to probe the effects of SARS-CoV-2 on those organs and screen drugs to treat the virus.
In the new study, the researchers first analyzed lung biopsies from COVID-19 patients and discovered that they had especially high levels of macrophages. To better understand the role of macrophages during a COVID-19 infection, Chen’s team developed an approach that could exploit the same line of human stem cells to become both lung cells and macrophages simultaneously. The fact that they arose from the same initial stem cells was important to prevent the immune cells from attacking the lung cells.
“This model system provides a perfect way to decode, step by step, how these three components—the immune system, the lungs, and the virus—interact,” said Chen.
A cascade of inflammation
When Chen’s lab infected the stem cell-derived lungs and macrophages with SARS-CoV-2, they found that not all macrophages responded in the same way. One subset, dubbed M2 macrophages, eliminate the virus by physically engulfing virus and virus-infected cells in a process known as phagocytosis, while releasing anti-inflammatory molecules.
M1 macrophages behaved in an opposite way: these cells released a plethora of inflammatory chemical signals that not only fight SARS-CoV-2, but cause a more widespread immune response. These same inflammatory factors have been shown to be present in the blood of people with severe COVID-19 symptoms.
“Our results suggest that people who already have M1 macrophages activated in the lungs when infected with COVID-19 might be more likely to develop very severe inflammation from the virus,” said Chen.
Elderly people and those with certain conditions like hypertension or diabetes—already known to be prone to more severe COVID-19 symptoms—may have higher levels of the M1 macrophages, she added.
Her team went on to show that antibodies—similar to those already used clinically to treat COVID-19—helped M2 macrophages clear the SARS-CoV-2 virus. More work is needed to show whether the observations hold true in humans, but the findings could help inform the prevention or treatment of severe COVID-19 in the most at-risk patients. And Chen is already thinking ahead to her next experiments with the stem cell-derived organoids.
“This model system is useful for decoding the molecular mechanisms behind not only COVID-19, but other infectious diseases,” said Chen.
In the future, her group hopes to make more complex mini-organs that include not only lung and immune cells, but blood vessels, nerves and other supporting cell types.
##
Journal
Nature
DOI
10.1038/s41467-022-29731-5
Article Title
Differential effects of macrophage subtypes on SARS-CoV-2 infection in a human pluripotent stem cell-derived model




