Geneva, March 30, 2023 – More than half of patients who suffer from chronic hepatitis B have the e antigen (HBeAg)-negative form of the disease. Even after many years of antiviral treatment with nucleos(t)ide analogues (NUC), lasting immune control is almost never seen. According to the current state of knowledge, those affected therefore require lifelong therapy. In the world’s first randomized controlled multicenter study – led by Leipzig University’s Faculty of Medicine and in partnership with the Centre for Clinical Studies (ZKS) – researchers have shown that many HBeAg-negative patients can achieve permanent immune control of hepatitis B if they discontinue antiviral therapy after a certain period of time. Their findings are published in the high-impact journal, the Journal of Hepatology.
Credit: Journal of Hepatology
Geneva, March 30, 2023 – More than half of patients who suffer from chronic hepatitis B have the e antigen (HBeAg)-negative form of the disease. Even after many years of antiviral treatment with nucleos(t)ide analogues (NUC), lasting immune control is almost never seen. According to the current state of knowledge, those affected therefore require lifelong therapy. In the world’s first randomized controlled multicenter study – led by Leipzig University’s Faculty of Medicine and in partnership with the Centre for Clinical Studies (ZKS) – researchers have shown that many HBeAg-negative patients can achieve permanent immune control of hepatitis B if they discontinue antiviral therapy after a certain period of time. Their findings are published in the high-impact journal, the Journal of Hepatology.
Hepatitis B is an inflammation of the liver caused by the hepatitis B virus that can lead to serious problems such as liver cirrhosis or liver cancer and is easily transmitted through body fluids. An estimated 350 million are chronically infected, making chronic hepatitis B one of the most common viral infections worldwide. People with chronic hepatitis B usually have to take antiviral medication for their entire life in order to reduce the viral load and normalize inflammation levels in the liver. Antiviral therapy consists of the administration of nucleoside or nucleotide analogues, which in patients with the HBeAg-negative form almost never leads to the permanent immune control that would allow the termination of treatment. The antiviral therapy is associated with high costs for the healthcare system and can cause serious side effects.
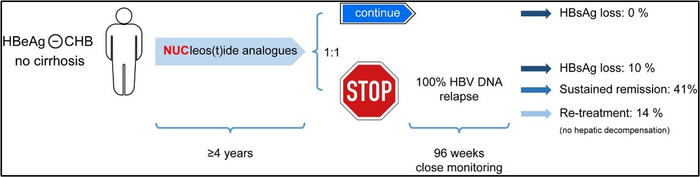
Results currently published in the Journal of Hepatology show in a study of 166 HBeAg-negative patients from 20 clinics across Germany that after 96 weeks of observation many patients who discontinued an effective antiviral treatment that they had taken for at least four years achieved immune control of the disease. In 10% of the patients, immune control was demonstrated through loss of previously detectable hepatitis B surface antigen (HBsAg) in the blood, an event which is considered a functional cure of hepatitis B.
By the end of the study, in about 41% of patients, hepatitis B virus levels in the blood were reduced to below the level of 2,000 units per millilitre, which according to international treatment guidelines means that there is no longer an indication for renewed antiviral therapy. Additionally, 77% of patients no longer had elevated liver inflammation levels. In contrast, no patient who continued antiviral treatment showed HBsAg loss.
Study leader Professor Florian van Bömmel, senior physician in the Department of Hepatology at Leipzig University Hospital said, “We were able to show that in some patients discontinuing long-term therapy with nucleoside or nucleotide analogues after at least four years is more effective than continuing it, and that many patients no longer require antiviral therapy at all after discontinuation. In particular, patients who show low HBsAg levels when they discontinue treatment have a high chance of functional cure.”
After discontinuation of treatment, all of the patients initially experienced a resurgence of hepatitis B virus replication and many also experienced transient renewed liver inflammation. Some patients with severe liver inflammation were then restarted on antiviral therapy to prevent liver damage. Patients with liver cirrhosis were not included in the study for safety reasons. No serious adverse events related to discontinuation of therapy occurred during the study. “However, in other studies, severe cases of hepatic inflammation were observed in a few cases after antiviral therapy was discontinued. Stopping NUC treatment should therefore only be carried out under the supervision of an experienced physician,” said the study leader.
Professor van Bömmel and Professor Thomas Berg, head of the Department of Hepatology at Leipzig University Hospital, are confident that the results of the STOP-NUC trial will have a major impact on the overall development of hepatitis B therapy: “We expect that in the future international guidelines for the treatment of hepatitis B will refer to this study. By the middle of this year, results from the extension of the study will be evaluated and will show whether the number of patients with immune control continues to increase in the long term after discontinuation of antiviral treatment.”
Journal
Journal of Hepatology
DOI
10.1016/j.jhep.2022.12.018
Method of Research
Randomized controlled/clinical trial
Subject of Research
People
Article Title
A multicenter randomized-controlled trial of nucleos(t)ide analogue cessation in HBeAg-negative chronic hepatitis B
Article Publication Date
28-Mar-2023




