Credit: The University of Hong Kong
Antimicrobial resistance posed by "superbugs" has been a major public health issue of global concern. Drug-resistant infections kill around 700,000 people worldwide each year. The figure could increase up to ten million by 2050, exceeding the number of deaths caused by cancers, according to figures of the World Health Organization (WHO).
Current clinical options for treating antibiotic resistant infections include increasing the prescribed antibiotic dose or using a combination therapy of two or more antibiotics. This might potentially lead to overuse of antibiotics, producing superbugs more resistant to antibiotics. Nevertheless, the development of antibiotic resistance far outruns the approvals of new antibacterial agents. While it may take a decade and cost an unusual high investment of USD 1 billion in average to bring a new drug to market, generating resistance to a new drug only requires a short couple of years by bacteria. Scientists and clinicians are in desperate need to discover an economic, effective, safe alternative strategy to meet the global public health challenge of antimicrobial resistance.
A research team led by Professor Sun Hongzhe of the Department of Chemistry, Faculty of Science and Dr Richard Kao Yi-Tsun of the Department of Microbiology, Li Ka Shing Faculty of Medicine, the University of Hong Kong (HKU) discovered an alternative strategy by repositioning colloidal bismuth subcitrate (CBS), an antimicrobial drug against Helicobacter pylori (H. pylori) -related ulcer.
They found the bismuth-based metallodrug to effectively paralyze multi-resistant superbugs, e.g. Carbapenem-resistant Enterobacteriaceae (CRE) and Carbapenem-resistant Klebsiella pneumoniae (CRKP) and significantly suppress the development of antibiotic resistance, allowing the lifespan of currently-used antibiotic to be largely extended. CRE and CRKP can cause deadly infections such as bacteremia, pneumonia, and wound infections.
The team is the first globally to link the "resistance-proof" ability of metallo-drug to the treatment of superbugs. This bismuth drug-based therapy looks set to become the last-line strategy against superbugs infections apart from development of new antibiotics. Since CBS is a US Food and Drug Administration (FDA)-approved drug, it will hopefully be rapidly ready for human clinical trials.
The findings were published in Nature Communications in January 2018 and a patent has been filed in the US for the discovery.
CRE is one of the three most dangerous superbugs on WHO's list of critical priority needs for new antibiotics. CRE resists almost all the clinically available antibiotics and spreads easily through person-to-person contact. If sepsis occurs, the death rate could be as high as 50%, according to the Centers for Disease Control (CDC) in the US.
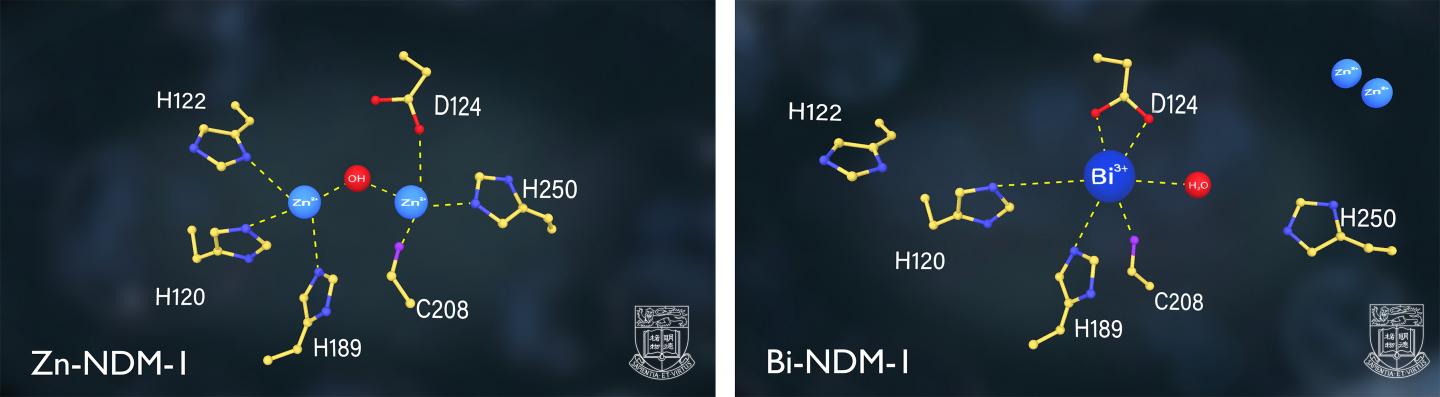
The research team found that CBS as well as other relevant bismuth-based compounds could serve as potent inhibitors of NDM-1 (New Delhi Metallo-β-lactamase 1), one of the leading resistant determinants that demonizes common bacteria into CRE superbugs. This enzyme inhabits in bacteria and arms them with resistance to almost all commonly used beta-lactam antibiotics including the so-called "last resort" Carbapenem.
The NDM-1 carrying CREs is lethal and extremely difficult to treat, which poses a great threat to public health and may drive the world to the cusp of a "post-antibiotic era". Scientists report that NDM-1 superbugs have now been disseminated to over 70 countries or regions across the world.
Through a series of tests on an NDM-1 Escherichia coli (E. coli) (denoted as NDM-HK), clinically collected by Dr Ho Pak Leung, Director of the HKU Carol Yu Centre for Infection, the team revealed that CBS can "tame" the superbug reducing it to almost sensitive strain which can be easily killed by commonly used Carbapenem antibiotics.
More importantly, the brand-new therapy allows the dose of antibiotics to be reduced by 90% to attain the same level of effectiveness, and the development of NDM-1 resistance to be significantly slowed down, which will largely extend the life cycle of currently used antibiotics.
In the mouse model of NDM-1 bacterial infection, combination therapy comprising CBS and Carbapenem significantly prolonged the life expectancy and raised the eventual survival rate of infected mice by more than 25 percentage points compared to Carbapenem monotherapy. The research team now concentrates on using CBS-based therapy in other animal infection models, e.g. urinary tract infection (UTI), hoping to offer a more extensive approach to combat with antibiotic resistant superbugs.
Dr Ho found the results very encouraging, he said: "There is currently no effective approach to overcome the NDM superbug. Bismuth has been used clinically for decades. Knowing that it can tame the NDM is like "a good rain after a long drought" for the scientific community."
Professor Sun said: "CBS has been clinically used for a long period of time in many countries and regions including Mainland China and Hong Kong, significantly enhances the eradication rate of resistant H. pylori. Surprisingly, no bismuth-resistant strain has been reported even after a long-term use. We hope CBS-based combination therapy will open up a new horizon for the treatment of infection caused by superbugs, serving as a new and more economical therapy to solve the problem of antimicrobial resistance (AMR)."
###
Media Contact
Melanie Wan
[email protected]
852-285-92600
http://www.hku.hk/
Original Source
https://www.hku.hk/press/news_detail_17499.html http://dx.doi.org/10.1038/s41467-018-02828-6