In a groundbreaking study published in BMC Pediatrics, researchers have explored the intricate relationship between serum levels of hypoxia-inducible factor 1-alpha (HIF-1α) and Bcl-2/adenovirus E1B 19-kDa interacting protein 3 (BNIP3) in pediatric patients who have experienced traumatic brain injury (TBI). This prospective cohort study focuses on how these serum markers correlate with injury severity and subsequent outcomes, highlighting their potential as critical indicators in clinical settings.
Traumatic brain injury in children has seen an alarming rise, necessitating immediate attention and innovative research methodologies. The complexity surrounding TBI outcomes in the pediatric population is multifaceted, influenced not just by the injury itself but also by biological markers in the patient’s system. The authors of the study, including researchers Yin, Meng, and Liu, have meticulously examined the trajectories of HIF-1α and BNIP3—markers that play significant roles in cellular response to injury and hypoxia.
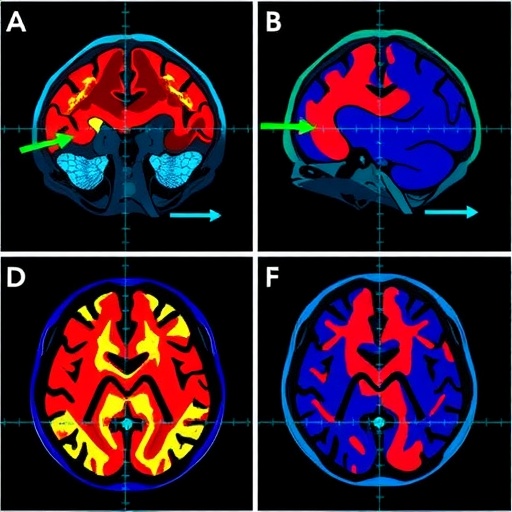
Understanding HIF-1α is crucial, as this transcription factor is pivotal in regulating the body’s response to low oxygen levels. Following a TBI, the brain requires a rapid response to manage oxygen deprivation and promote neuronal survival. HIF-1α facilitates the activation of various genes that contribute to angiogenesis, metabolism, and survival under hypoxic conditions, making it a potential biomarker for assessing injury severity in TBI cases.
BNIP3, on the other hand, is associated with autophagy and programmed cell death, also known as apoptosis. This aspect of cellular biology is incredibly relevant because, following a traumatic injury, the fate of neurons can hinge on these processes. Elevated levels of BNIP3 post-injury might indicate a shift toward cell death rather than recovery, suggesting poor outcomes for the patient. This study aims to link the levels of these proteins in serum with the clinical trajectories of pediatric TBI patients, creating a foundation for improved prognostic assessments.
The researchers collected data from a carefully selected cohort of pediatric patients who suffered varying degrees of TBI. By measuring serum levels of HIF-1α and BNIP3 when the patients were admitted to the hospital and then tracking these levels over time, the researchers were able to establish patterns that correlate with injury severity. This approach required a sophisticated analysis to ensure that the confounding factors, such as age, gender, and pre-existing conditions, were accounted for, thereby lending credibility to the findings.
What makes this study particularly noteworthy is its prospective design, which allows for a real-time assessment of biomarker trajectories. Unlike retrospective studies, which rely on past events, the prospective nature provides fresh insights into how serum levels change in response to therapeutic interventions and the biological healing processes. This methodological strength enhances the reliability of results and supports the call for continuous monitoring of these biomarkers in clinical practice.
The implications of the findings are far-reaching. If further studies can validate the use of HIF-1α and BNIP3 as reliable biomarkers for pediatric TBI, this could pave the way for new diagnostic and treatment protocols that are tailored specifically to children. This could lead to timely interventions that target adverse biological responses following traumatic brain injuries, thus improving recovery outcomes and reducing long-term disabilities.
The stark realities of pediatric TBI cannot be overstated, as many children suffer from lifelong disabilities due to such injuries. Current treatment protocols often fail to account for individual biological variations in patients, leading to a one-size-fits-all approach that may not be effective for every child. The findings from this study advocate for a more personalized medicine approach, where treatment plans are informed by real biological markers that indicate recovery trajectories.
This research was also set within a larger discourse on the importance of precision medicine in treating pediatric populations. The ability to use serum biomarkers to predict outcomes could significantly enhance patient care strategies, enabling clinicians to monitor patients more proactively and intervene when necessary.
The study has garnered interest from various quarters, including medical professionals, researchers, and advocacy groups focused on pediatric health issues. The potential to identify at-risk children based on serum readings could revolutionize the standards of care for acute brain injuries in young patients, leading to better resource allocation and targeted therapeutic approaches.
In conclusion, the work undertaken by Yin, Meng, and Liu represents a significant contribution to the field of pediatric neurology and trauma medicine. As researchers continue to delve into the mechanisms underlying TBI and its aftermath, the integration of serum biomarker analysis into clinical practice seems to be an emerging frontier with the potential to transform patient outcomes dramatically.
As we continue to advocate for the advancement of research in pediatric TBI, it is essential to recognize the value of integrating clinical practices with the latest scientific findings. This study serves as a reminder that solutions to complex medical challenges are often found at the intersection of innovative research and compassionate care.
The medical community is urged to consider the findings of this study, as the pathways open up numerous avenues for research and clinical improvement. With ongoing advancements, the hope is that future pediatric patients suffering from traumatic brain injuries will benefit from these insights, ultimately leading to fewer long-term repercussions of their injuries.
As we reflect on these outcomes, we are reminded that trauma does not just affect the brain; it influences lives, families, and futures. With ongoing research efforts such as this, there is optimism for a brighter future for children affected by traumatic brain injuries.
Subject of Research: Pediatric Traumatic Brain Injury and Serum Biomarkers
Article Title: Trajectories of serum HIF-1α and BNIP3 are associated with injury severity and outcomes in pediatric traumatic brain injury: a prospective cohort study.
Article References:
Yin, H., Meng, Lj., Liu, Kx. et al. Trajectories of serum HIF-1α and BNIP3 are associated with injury severity and outcomes in pediatric traumatic brain injury: a prospective cohort study.
BMC Pediatr (2026). https://doi.org/10.1186/s12887-026-06528-9
Image Credits: AI Generated
DOI: 10.1186/s12887-026-06528-9
Keywords: pediatric TBI, HIF-1α, BNIP3, biomarkers, injury severity, clinical outcomes.
Tags: angiogenesis and neuronal survivalBNIP3 as biomarkercellular response to brain injuryclinical indicators for TBIHIF-1α serum levelshypoxia-inducible factors in TBIinjury severity and biomarkersinnovative methodologies in TBIpediatric health researchpediatric traumatic brain injuryprospective cohort study on TBITBI outcomes in children