In a groundbreaking advancement that could revolutionize cancer research and therapeutic development, a team of scientists led by Mocellin, Treillard, and Robinson has unveiled an innovative microfluidic platform designed to model hepatocellular carcinoma (HCC) and its complex microenvironment within a chip. Published in 2025 in Cell Death Discovery, this study presents a sophisticated organ-on-a-chip model that mimics the tumor’s intricate biology with unprecedented precision. This breakthrough holds the promise of transforming how researchers investigate liver cancer, offering a highly controllable, reproducible, and physiologically relevant system that surpasses traditional in vitro models and animal studies.
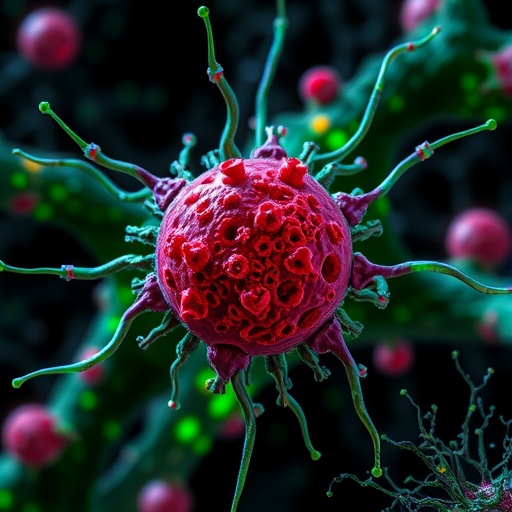
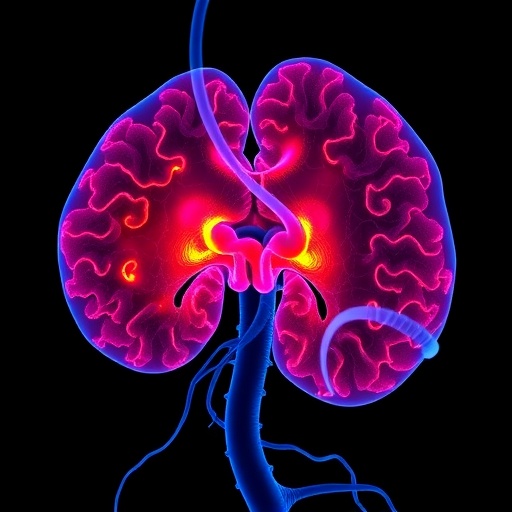
Hepatocellular carcinoma remains one of the deadliest cancers worldwide due to its aggressive nature and limited treatment options. One of the critical challenges in studying HCC has been the inability to faithfully replicate the tumor’s microenvironment ex vivo, which includes not only cancer cells but also surrounding stromal cells, immune components, and the extracellular matrix milieu. Traditional two-dimensional culture systems fail to offer the spatial and biochemical complexity required to understand tumor-stroma interactions, immune modulation, and drug responses. The newly developed microenvironment-on-a-chip overcomes these obstacles by integrating multiple cell types within a dynamically perfused microfluidic device that recapitulates HCC’s structural and functional attributes.
At its core, the chip technology advances beyond static culture by introducing a finely tuned microfluidic network that simulates blood flow conditions, enabling nutrient and oxygen gradients similar to those found in vivo. This feature is crucial since tumor hypoxia and metabolic heterogeneity significantly influence HCC progression and therapeutic resistance. By incorporating liver-specific endothelial cells, stellate cells, and immune cells alongside carcinoma cells, the model allows for real-time assessment of cellular crosstalk under physiologically relevant shear stress and chemical gradients. Such dynamic interactions are pivotal in tumor growth, angiogenesis, and immune evasion.
The study highlights detailed characterization of the tumor microenvironment simulated on the chip, including extracellular matrix remodeling and cytokine profiles characteristic of liver malignancies. Using high-resolution imaging and transcriptomic analyses, the researchers verified that the tumor cells on-chip expressed hallmark molecular signatures of HCC and exhibited phenotypic behaviors such as invasiveness and proliferation rates comparable to clinical observations. Intriguingly, immune cell infiltration patterns were also faithfully mirrored, providing novel insights into the tumor-immune interface that are difficult to capture with conventional models.
By harnessing this technology, researchers demonstrated the ability to simulate and dissect the multifaceted responses of HCC tumors to various chemotherapeutic agents and immunotherapies. Rather than relying on static endpoint measurements, the chip enables longitudinal monitoring of drug efficacy and resistance evolution by tracking changes in cell viability, migration, and secretome dynamics over time. This capability ushers in a new era of personalized medicine approaches for liver cancer, where treatments can be tailored and optimized using patient-derived cells within these microengineered platforms.
Incorporating patient-specific biopsies into the organ-on-a-chip system opens doors for precision oncology applications. It empowers clinicians and researchers to generate bespoke tumor models that account for genetic and epigenetic heterogeneity, ultimately predicting individual patient responses to therapy with a level of accuracy unattainable by current preclinical models. Moreover, the scalability of the chip design promises potential for high-throughput drug screening, accelerating the discovery of novel anticancer compounds and combination regimens that are effective against resistant HCC subtypes.
The integration of microengineering, cell biology, and computational modeling was critical to the success of this platform. Sophisticated design considerations ensured optimal cell compartmentalization, mechanical properties consistent with hepatic tissue, and modulation of biochemical signaling pathways to authentically mimic the chronic inflammatory and fibrotic cues that often accompany hepatocellular carcinoma development. These technical refinements reflect a maturation of organ-on-a-chip technology from proof-of-concept to application-ready systems in cancer biology.
Furthermore, the microfluidic chip also facilitates exploration of metastasis and cancer stem cell niches within HCC. By manipulating spatial configurations and fluid shear forces, the study elucidates mechanisms by which tumor cells detach, invade surrounding matrices, and potentially intravasate into bloodstream analogs within the device. Understanding these steps under controlled conditions lays foundational work for strategic intervention points that may inhibit HCC dissemination and improve patient prognoses.
The multidisciplinary approach adopted by the authors merges experimental data with computational analyses of signaling networks, metabolic fluxes, and immune cell dynamics, paving the way for predictive modeling of tumor evolution and therapeutic outcomes. These insights provide a systems-level perspective crucial for designing next-generation therapeutics that target not just tumor cells, but the entire ecosystem that sustains malignancy and mediates drug resistance.
Importantly, this development addresses ethical and logistical drawbacks of animal models by providing human-relevant results without the complexity and variability often seen in in vivo systems. This paradigm shift aligns with global efforts to reduce animal testing and enhance translational fidelity from bench to bedside, ultimately accelerating clinical advancements for HCC patients worldwide.
Looking forward, the authors suggest that continued refinement of the model—including integration of vasculature-on-a-chip components, immune checkpoint modulations, and real-time biosensors—could further elevate the platform’s utility. Such enhancements will enable comprehensive dissection of therapeutic mechanisms, synergy effects, and emergent resistance patterns with temporal resolution previously unattainable, heralding a transformative era in cancer research.
This microenvironment-on-a-chip represents not only a technological triumph but also a conceptual leap in oncology, fundamentally redefining how complex liver tumors can be studied in controlled yet biologically faithful settings. The convergence of this platform with personalized medicine, high-throughput screening, and computational oncology promises to deliver breakthroughs in diagnosis, prognosis, and treatment strategies that save lives and improve quality of life for millions affected by hepatocellular carcinoma.
In light of these findings, the broader scientific community is poised to embrace organ-on-chip systems as indispensable tools for studying tumor biology. As the study by Mocellin and colleagues demonstrates, bridging the gap between microengineering and cancer biology opens fertile ground for innovation with profound clinical implications.
Ultimately, this advance underscores the vital importance of interdisciplinary collaboration to tackle the formidable challenge presented by hepatocellular carcinoma—a malignancy notorious for its complexity and therapeutic intractability. With sustained research and development spurred by this new model, a future where HCC can be routinely studied, understood, and effectively managed at the individual patient level draws increasingly near.
Subject of Research: Modeling hepatocellular carcinoma and its tumor microenvironment using organ-on-a-chip technology.
Article Title: Modeling hepatocellular carcinoma and its microenvironment on a chip.
Article References:
Mocellin, O., Treillard, S., Robinson, A. et al. Modeling hepatocellular carcinoma and its microenvironment on a chip.
Cell Death Discov. (2025). https://doi.org/10.1038/s41420-025-02917-8
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02917-8
Tags: advanced cancer research techniquescancer microenvironment modelingdrug response in HCCex vivo tumor modelinghepatocellular carcinoma researchimmune modulation in cancerinnovative cancer research methodologiesliver cancer therapeutic developmentmicrofluidic device for cancerorgan-on-a-chip technologyprecision cancer therapiestumor-stroma interactions