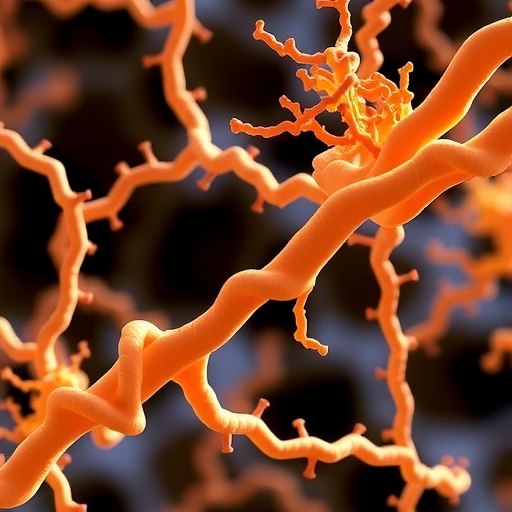
In a groundbreaking advancement poised to transform the treatment landscape for lysosomal storage disorders, a team of researchers has unveiled a novel therapeutic strategy that effectively ameliorates both the neuropathology and behavioral deficits in a mouse model of mucopolysaccharidosis IIIB (MPS IIIB). This rare genetic disorder, characterized by profound deficiency in the enzyme α-N-acetylglucosaminidase, leads to the accumulation of heparan sulfate and subsequent devastating neurological deterioration. The latest study, published in Cell Death Discovery, introduces an innovative approach involving heparan sulfate binding proteins, highlighting their remarkable capacity to mitigate disease progression at both molecular and behavioral levels.
Mucopolysaccharidosis IIIB, part of the mucopolysaccharidoses spectrum, manifests primarily through severe neurodegeneration due to lysosomal storage malfunction. The disease pathology arises when neurons accumulate undegraded glycosaminoglycans, triggering widespread cellular stress, inflammation, and cell death. Traditional therapies have struggled to penetrate the blood-brain barrier effectively or to alter the central nervous system pathology, rendering MPS IIIB an almost invariably fatal childhood condition. Addressing this challenge, the researchers investigated the therapeutic potential of proteins exhibiting high affinity for heparan sulfate, the dysfunctional substrate in MPS IIIB.
Central to the study was the utilization of a heparan sulfate binding protein (HSBP) treatment designed to sequester the excessive glycosaminoglycans, thus preventing their pathological accumulation and the cascade of downstream neurotoxic effects. Administered to MPS IIIB mice, these proteins demonstrated robust engagement with accumulated heparan sulfate, promoting its clearance and reducing lysosomal stress. The intervention led to pronounced suppression of inflammatory markers and apoptotic signals within affected brain regions, signifying a direct neuroprotective impact uncommon in prior therapeutic attempts.
.adsslot_WPd3t6rUzG{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_WPd3t6rUzG{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_WPd3t6rUzG{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Delving deeper into the neuropathological outcomes, the team observed substantial improvements in neuronal architecture and function post-treatment. Histological analyses revealed diminished lysosomal enlargement and reduced presence of pro-inflammatory microglia, indicators of halted disease progression. Notably, quantitative assessments demonstrated attenuation of hippocampal and cortical neuron loss, regions critically involved in memory and cognition, underlining the treatment’s potential to preserve vital neural circuits compromised in MPS IIIB patients.
Behavioral assays conducted concomitantly with neuropathological evaluations uncovered striking reversal of motor deficits and cognitive impairments in treated animals. Untreated MPS IIIB mice exhibited pronounced hyperactivity, impaired spatial memory, and anxiety-like behaviors, all hallmarks of the human condition. Treatment with HSBP normalized locomotor activity and restored performance in maze navigation tests, reflecting tangible improvements in neurological function that correlate with the observed cellular restoration.
At the molecular level, the study illuminated the multifaceted mechanisms by which heparan sulfate binding proteins facilitate therapeutic effects. By directly binding accumulated glycosaminoglycans, HSBPs not only reduce lysosomal burden but also indirectly modulate extracellular matrix interactions and mitigate aberrant cell signaling. This multifactorial approach contrasts sharply with monotherapy enzyme replacement or gene therapy, often limited by the complexity of lysosomal biology and intracellular trafficking impediments in neurodegenerative diseases.
Importantly, the pharmacokinetic profile of the HSBP therapy indicated efficient brain penetration and sustained retention, attributes critical for successful CNS-targeted treatments. The researchers employed advanced protein engineering to optimize molecular size and charge, enhancing blood-brain barrier transcytosis without eliciting immune reactions, addressing key hurdles that have historically thwarted lysosomal enzyme therapies for neuropathic mucopolysaccharidoses.
Translational relevance of these findings is further reinforced by the comprehensive safety evaluation accompanying efficacy results. Treated mice exhibited no signs of systemic toxicity or detrimental off-target effects over prolonged treatment periods. Biomarkers for hepatic and renal function remained within normal limits, suggesting a favorable therapeutic index that could accelerate clinical development pipelines.
This pioneering therapeutic concept also opens the door to combinatorial strategies, where HSBP treatment could be integrated with existing enzyme replacement or gene therapies to enhance efficacy. By lowering pathological substrate accumulation extracellularly while restoring enzymatic function intracellularly, a synergistic effect may prove transformative for MPS IIIB and related disorders marked by glycosaminoglycan dysregulation.
Beyond mucopolysaccharidosis IIIB, the implications of this work resonate with broader neurodegenerative research fields. Excessive heparan sulfate accumulation and proteoglycan dysregulation have been implicated in diseases like Alzheimer’s and Parkinson’s, suggesting that heparan sulfate binding proteins may have wider applicability. Future exploratory studies could unveil their potential in modulating proteopathic aggregates and neuroinflammatory processes across diverse neuropathologies.
The study also discusses the potential refinement of dosing regimens and administration routes, with intrathecal delivery posing as a promising conduit for maximizing CNS bioavailability while minimizing peripheral exposure. Such approaches may fine-tune therapeutic impact, enhancing precision medicine applications tailored to individual patient needs and disease severity profiles.
Moreover, biophysical characterization of the interaction between HSBPs and glycosaminoglycans provided insight into drug design parameters crucial for optimizing binding affinity and specificity. These structural studies underpin next-generation protein engineering efforts aimed at creating even more potent and durable therapeutics, capitalizing on the modular nature of heparin-binding domains.
In summary, this landmark research illuminates a novel avenue in the treatment of a formerly intractable neurodegenerative disease. The strategic use of heparan sulfate binding proteins to combat substrate buildup marks a paradigm shift, with clear demonstrable benefits on neuronal integrity and function in preclinical models. As the field advances, translation to human clinical trials could redefine therapeutic standards and hope for MPS IIIB patients worldwide.
Continued interdisciplinary collaboration between molecular biologists, neurologists, and pharmacologists will be essential to refine these promising therapies. Comprehensive longitudinal studies will evaluate long-term efficacy and potential disease-modifying capabilities, marking critical milestones towards regulatory approvals and eventual patient access.
Ultimately, this study exemplifies the power of biochemically targeted therapeutics designed from molecular pathogenesis insights, heralding a future where devastating genetic neurological conditions may be effectively controlled or even reversed. The intersection of cutting-edge protein engineering and neurodegenerative disease biology has never been more promising or inspiring.
Subject of Research: Therapeutic intervention targeting neuropathology and behavioral abnormalities in mucopolysaccharidosis IIIB using heparan sulfate binding proteins.
Article Title: Heparan sulfate binding protein treatment ameliorates neuropathology and behavioral abnormalities in mucopolysaccharidosis IIIB mice.
Article References:
Anzilotti, S., Scarcella, M., Ciampa, M. et al. Heparan sulfate binding protein treatment ameliorates neuropathology and behavioral abnormalities in mucopolysaccharidosis IIIB mice. Cell Death Discov. 11, 362 (2025). https://doi.org/10.1038/s41420-025-02648-w
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02648-w
Tags: blood-brain barrier challengesCell Death Discovery publicationdisease progression mitigationglycosaminoglycan accumulationheparan sulfate binding proteinsHeparan sulfate protein therapyinnovative therapeutic strategieslysosomal storage disorders researchMucopolysaccharidosis IIIB treatmentneurodegeneration in childhood diseasesneuropathology and behavioral deficitsα-N-acetylglucosaminidase deficiency