In a groundbreaking study exploring the intricate landscape of healthcare utilization among Asian origin groups, researchers led by Vu et al. present compelling findings that highlight the significant variations in access to and usage of healthcare services based on citizenship status. As the global population becomes increasingly diverse, understanding these disparities is pivotal for developing inclusive healthcare policies. The study sheds light on how cultural factors, immigration status, and systemic barriers intertwine, affecting the well-being of these communities.
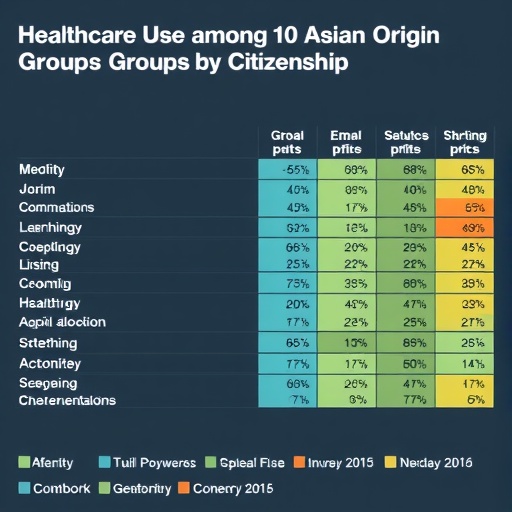
The research draws on a comprehensive analysis that encompasses a range of Asian origin groups, providing insights into their unique healthcare needs and challenges. This nuanced perspective is crucial as it challenges the monolithic view often associated with Asian populations. By disaggregating data among various subgroups, the authors illuminate the distinct health trajectories influenced by factors such as language barriers, financial constraints, and varying degrees of familiarity with the healthcare system based on legal status.
Interestingly, citizenship status has emerged as a critical determinant in healthcare access. The differential treatment experienced by citizens versus non-citizens or undocumented individuals is not merely a matter of eligibility for services but reflects deeper systemic inequities. The researchers note that many immigrants grapple with fear and uncertainty regarding their legal status, leading to avoidance of medical care. This avoidance can have dire consequences, including untreated chronic illnesses and worsened health conditions, highlighting an urgent need for policy interventions.
Moreover, the study underscores the importance of culturally competent healthcare services. Many Asian origin groups possess distinct cultural beliefs about health and wellness that can affect their interaction with healthcare systems. The findings suggest that healthcare providers must be trained to recognize and respect these cultural differences to bridge the gap in care provision. Creating an environment where patients feel understood and supported may encourage higher utilization rates, ultimately leading to improved health outcomes.
The research methodology employed by Vu et al. is both robust and comprehensive, utilizing a mixture of qualitative and quantitative approaches. Surveys, interviews, and focus groups were conducted across various communities to gather diverse perspectives. Such methodological pluralism enriches the data and facilitates a deeper understanding of core issues. By employing mixed methods, the authors not only capture statistical trends but also bring forth personal narratives that humanize the data, making it more relatable and actionable.
As policymakers grapple with the pressing need for healthcare reform, the findings of this study advocate for targeted initiatives that address the distinct challenges faced by Asian origin groups. The authors propose collaborative approaches involving community organizations and healthcare providers to enhance outreach and education. Such partnerships can foster trust and empower individuals to seek necessary medical assistance without fear of repercussions.
Furthermore, the implications of this study extend beyond healthcare access and into the realm of public health. Researchers are increasingly recognizing that social determinants of health—such as housing, education, and employment—play a significant role in health outcomes. The barriers identified in Vu et al.’s research highlight a larger societal issue that warrants attention from both healthcare providers and policymakers alike.
In addressing the pressing issues of healthcare utilization among Asian origin groups, the study also emphasizes the need for longitudinal research to track changes over time. Understanding the evolving dynamics of healthcare access as immigration patterns shift is crucial for anticipating future healthcare needs. This dynamic perspective will enable more effective planning and resource allocation within healthcare systems.
The importance of institutional support cannot be overstated. The authors call for healthcare facilities to implement policies that specifically cater to the needs of non-citizen populations. This could include language services, financial assistance programs, and navigational resources that guide individuals through the healthcare system. By reducing barriers to access, healthcare providers can work towards bridging the gap that currently exists in care delivery.
As the conversation surrounding healthcare continues to evolve, the findings of Vu et al. serve as a rallying cry for inclusive practices that embrace diversity. The authors posit that healthcare is a fundamental human right, and ensuring equitable access is vital for the overall health of society. This study contributes significantly to the discourse on health equity, urging stakeholders across sectors to join forces in addressing systemic disparities.
Public awareness plays a crucial role in changing perceptions and reducing stigmas surrounding healthcare for immigrant populations. The authors encourage advocacy efforts that highlight the unique challenges faced by different Asian origin groups. By fostering a more informed public, the potential for policy change grows, as elected officials recognize the pressing needs of their constituents.
In summary, Vu et al.’s comprehensive examination of healthcare utilization among Asian origin groups serves as a vital resource for understanding the intricate web of factors that influence health access. The interplay between citizenship status, cultural beliefs, and systemic barriers underscores the importance of a tailored approach to healthcare delivery. This research not only identifies areas requiring immediate attention but also lays the groundwork for future studies aimed at enhancing health equity across diverse populations.
The call to action is clear: it is imperative for healthcare systems to evolve in response to the diverse needs of immigrant populations. By prioritizing inclusivity and awareness, stakeholders can create a healthcare landscape that is accessible, equitable, and just for all individuals, regardless of their origin or legal status.
Subject of Research: Utilization of Healthcare Among Asian Origin Groups and Citizenship Status
Article Title: Utilization of Healthcare Among Asian Origin Groups and Citizenship Status
Article References:
Vu, M., Nielson, M.K., Bui, L.N. et al. Utilization of Healthcare Among Asian Origin Groups and Citizenship Status.
J GEN INTERN MED (2025). https://doi.org/10.1007/s11606-025-10066-y
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11606-025-10066-y
Keywords: Healthcare, Utilization, Asian Origin Groups, Citizenship Status, Health Equity, Systemic Barriers, Cultural Competence, Social Determinants of Health.
Tags: Asian origin healthcare utilizationcitizenship status and health servicescultural factors in healthcare accessdisaggregated data in health researchfinancial constraints in healthcare accesshealthcare access disparitieshealthcare challenges for Asian communitiesimmigrant health and well-beinginclusive healthcare policy developmentlanguage barriers in healthcarenon-citizen healthcare experiencessystemic barriers in immigrant health