Credit: B. D. Colen/Harvard University
Harvard researchers have created a new, greatly simplified, platform for antibiotic discovery that may go a long way to solving the crisis of antibiotic resistance.
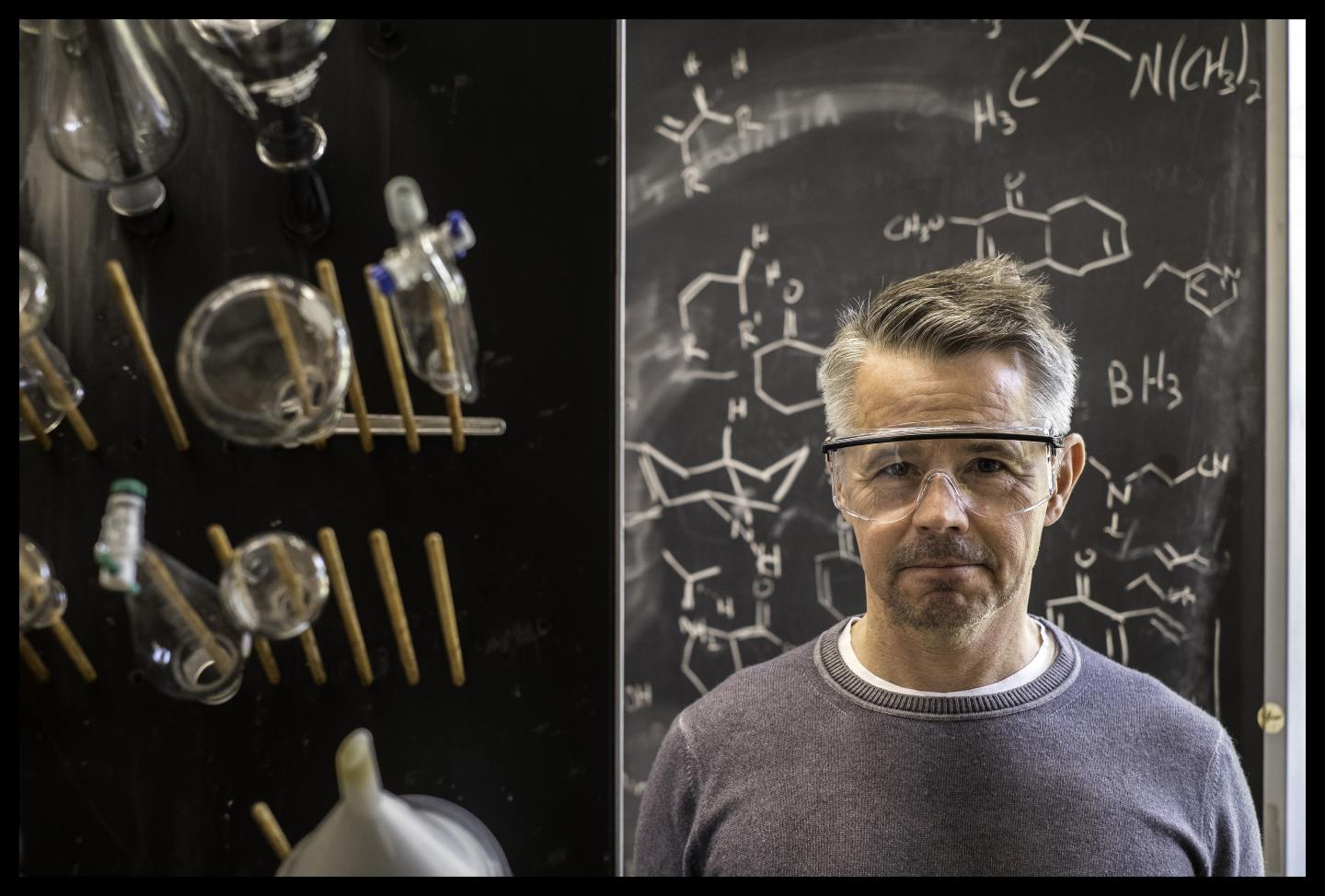
In a study just published in the journal Nature, Andrew G. Myers and colleagues describe "a platform where we assemble eight (chemical) building blocks by a simple process to make macrolide antibiotics" without using erythromycin, the original macrolide antibiotic, and the drug upon which all others in the class have been based since the early 1950s.
Erythromycin, which was discovered in a soil sample from the Philippines in 1949, has been on the market as a drug by 1953. "For 60 years chemists have been very, very creative, finding clever ways to 'decorate' this molecule, making changes around its periphery to produce antibiotics that are safer, more effective, and overcome the resistance bacteria have developed," says Myers, Amory Houghton Professor of Chemistry and Chemical Biology in Harvard's Department of Chemistry and Chemical Biology. "That process is semisynthesis, modifying the naturally occurring substance."
In contrast, the process described in the Nature study involves using "eight industrial chemicals, or substances derived from them," Myers says, and manipulating them in various combinations and then testing the products against panels of disease causing bacteria. This allows us to make new "new compounds in fewer steps than was previously possible."
Ian H. Seipel, who was a post doctoral fellow in Myers's lab and now is at the School of Pharmacy at UC San Francisco, and Ziyang Zhang, a Myers post doc, are first author's on the Nature report.
For a host of reasons – from the difficulty of developing antibiotics to the relatively low return on investment they offer, by 2013 the number of international pharmaceutical companies developing antibiotics had dwindled to four. And in each five year period from 1983 through 2007, the number of new antibiotics approved for use in the US decreased, from 16 at the beginning of that period to only five by its end.
One thing that has complicated antibiotic development is a perceived reluctance by federal agencies to fund the research. In fact, Myers says, his new antibiotic development system would have been impossible without support from a Harvard alum and his wife who are interested in science, and Harvard's Blavatnik Accelerator Fund, which provided support for the initial creation of Myers's company Macrolide Pharmaceuticals.
"I was making a presentation to a group of visiting alumns interested in science and one, Alastair Mactaggart, asked me about funding. I told him I had no funding – because at that time we didn't, and he followed me back to my office and said, 'this is ridiculous: we have to do something about this.'" Myers said that without the support of MacTaggart and his wife, Celine, and the Gustavus and Louise Pfeiffer Research Foundation, the new antibiotic creation platform would not exist. "And the Blavatnik Accelerator funding was also hugely important."
The Blavatnik Biomedical Accelerator awarded funding to Myers' project in 2013, enabling synthesis and testing of compounds. In 2015, with support from Harvard's Office of Technology Development, Myers founded a startup, Macrolide Pharmaceuticals, which has licensed the synthesis platform and aims to commercialize novel antibiotics for serious infections.
"One of the things that's quite encouraging about the data in our paper is that some of the structures we've made are active against clinical bacterial strains that are resistant to every known macrolide," Myers said. In fact, he added, two of the 350 compounds reported on in the Nature paper have, in initial testing, shown efficacy against a bacterium that has become resistant to vancomycin, "which is known as the antibiotic of last resort. And if you have a bug that's resistant to vancomycin, you're in trouble," Myers adds.
"This is an early effort," Myers says of his lab's work with the new drug development system. "We have a lot of work ahead of us." Some of the 350 compounds reported on in the paper will undergo more extensive testing to evaluate their potential as candidate drugs.
Myers is quick to point out that the road from drug candidate to a treatment at the bedside is long, arduous, and expensive. First comes the initial identification of possible compounds. "Microbiologists evaluate those against panels of bacteria," explains Myers. "Hopefully your panels contain clinically relevant strains that are found in hospitals. "If you find an effective compound, then you advance it: First you make sure it's not toxic to human cells in the lab; then you see how stable it is in human plasma; next come animal studies – typically in rodents to see if you can cure infection. And then come the three phases of human studies.
"I said to a friend the other day," says Andrew Myers, "that I'm really pleased this paper is out – my students worked unbelievably hard to make this happen. But if this is where this ends, I won't be satisfied. Our objective from day one was to have a drug in the clinic."
###
Media Contact
B. D. Colen
[email protected]
617-413-1224
@HarvardResearch
http://www.harvard.edu