In a groundbreaking advancement poised to redefine our understanding of cardiovascular physiology, researchers have unveiled a novel mechanism through which the hormone glucagon-like peptide-1 (GLP-1) confers cardioprotection. The study, recently published in Nature Communications, elucidates how GLP-1 activates ATP-sensitive potassium (K_ATP) channels in coronary pericytes, cells traditionally overshadowed by cardiomyocytes and endothelial cells in heart research. This intricate signaling axis, bridging the brain, gut, and heart, highlights a sophisticated biological dialogue that may pave the way for transformative therapies targeting heart disease.
GLP-1, best known for its roles in glucose metabolism and appetite regulation, has now been spotlighted as a pivotal mediator in cardiovascular health. Beyond its endocrine functions, GLP-1 appears to orchestrate a protective cascade within the coronary microvasculature by acting upon pericytes—contractile cells enveloping capillaries and small vessels—thereby modulating myocardial blood flow. The activation of K_ATP channels within these pericytes emerges as a critical effector step, suggesting a hitherto unappreciated layer of metabolic and vascular integration facilitating cardioprotective outcomes.
At the heart of this discovery lies the concept of brain-gut-heart signaling, an intersection of neuroendocrine and cardiovascular biology that exemplifies the body’s systemic interconnectivity. Prior to this research, the protective effects of GLP-1 on the heart were largely attributed to its direct impact on cardiomyocytes or systemic metabolic improvements. However, Mastitskaya and colleagues pivot attention to the microvascular milieu, uncovering how neuronal inputs modulate gut hormone release, which in turn influences coronary microcirculatory dynamics through pericyte K_ATP channel activation. This paradigm shift reframes cardioprotection as a multisystemic event rather than a solely cardiac-intrinsic phenomenon.
Technically, the researchers employed a combination of sophisticated electrophysiological assays, high-resolution imaging, and genetically modified animal models to delineate the cellular and molecular pathways involved. Functional studies demonstrated that GLP-1 receptor activation on coronary pericytes induces K_ATP channel opening, leading to hyperpolarization and reduced cellular contractility. This relaxation of pericytes facilitates capillary dilation, enhancing perfusion to myocardial tissue, particularly under stress conditions such as ischemia. The implications of improved microvascular flow are profound, as they provide a mechanism through which GLP-1 agonists might mitigate ischemic injury and potentially improve outcomes after myocardial infarction.
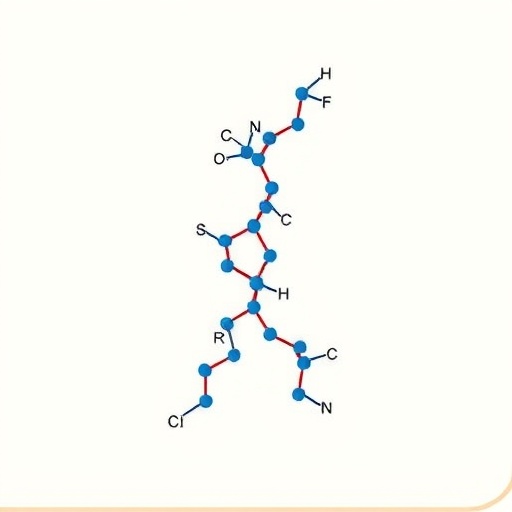
Delving deeper into the cellular machinery, the study highlights the importance of K_ATP channels as metabolic sensors, coupling the energetic state of the cell to membrane potential and contractile function. These channels, formed by inward-rectifier potassium channel subunits and regulatory sulfonylurea receptors, respond to intracellular nucleotide levels, thus serving as gatekeepers aligning cellular activity with metabolic demands. GLP-1’s capacity to activate these channels via receptor-mediated signaling pathways underscores a novel metabolic checkpoint in coronary pericytes that fine-tunes myocardial perfusion in real time.
Of particular interest is the elucidation of receptor signaling cascades linking GLP-1 receptor engagement to K_ATP channel activation. The study indicates a complex interplay involving cyclic AMP (cAMP) as a second messenger, protein kinase A (PKA) activation, and potential modulation of channel phosphorylation states. These signal transduction events exemplify the intricacy of hormone-channel communication and suggest additional molecular targets for therapeutic exploitation. Importantly, these pathways may offer opportunities to enhance or mimic endogenous cardioprotective mechanisms through pharmacological agents.
The involvement of pericytes as essential mediators in this context also revisits their functional significance within the coronary microvasculature. Traditionally regarded as supportive structural elements or regulators of blood-brain barrier integrity, pericytes emerge here as dynamic regulators of coronary flow and cardiac resilience. Their contractile ability, governed by ion channel activity, positions them uniquely at the interface of neurohumoral signaling and vascular response. This insight redefines pericyte biology and sparks new interest in their role within cardiovascular pathophysiology.
Moreover, the brain-gut-heart axis delineated in this research emphasizes systemic integration over isolated organ function. Neural circuits modulating GLP-1 secretion from enteroendocrine L-cells in the gut link central nervous system activity to cardiac outcomes via endocrine effectors. Such integration elucidates how acute and chronic stress responses, metabolic status, and neurohumoral signals converge to influence myocardial perfusion and survival. This multidimensional perspective demands a reevaluation of therapeutic strategies, advocating for holistic approaches that transcend individual organ systems.
Clinically, the ramifications are vast. GLP-1 receptor agonists, already established as treatments for type 2 diabetes and obesity, could be repurposed or optimized to exploit this cardio-coupling mechanism. Their ability to activate coronary pericyte K_ATP channels provides a mechanistic rationale for observed reductions in cardiovascular events in patients treated with these agents. Furthermore, targeted modulation of pericyte function might offer new avenues for protecting the myocardium in vulnerable populations, such as those with ischemic heart disease or heart failure.
This revelation also opens paths for biomarker discovery, with changes in pericyte function or K_ATP channel activity potentially serving as indicators of cardiovascular health or treatment efficacy. Advances in imaging techniques and molecular diagnostics could enable non-invasive monitoring of this signaling axis, guiding personalized interventions and improving prognostication.
From a broader scientific perspective, the identification of the GLP-1-K_ATP channel axis provides a platform for future research into microvascular biology and metabolic regulation. Other hormones or neurotransmitters may similarly influence pericyte function, indicating a generalizable principle of neuroendocrine control over capillary dynamics. Understanding these pathways could uncover novel mechanisms underpinning various cardiovascular and systemic diseases.
The methodology employed by Mastitskaya et al. showcases the power of interdisciplinary research, combining molecular biology, physiology, and advanced imaging to untangle complex biological systems. Their integrative approach sets a benchmark for future investigations into subtle yet impactful cellular mechanisms that govern organ system resilience and adaptability.
As the field advances, potential challenges arise, including delineating the long-term effects of chronic GLP-1 stimulation on pericytes and ensuring that therapeutic strategies avoid undesirable vascular side effects. Careful balance will be necessary to harness the benefits of K_ATP channel activation without compromising vascular integrity or function.
Yet, the promise is undeniable. This study provides a compelling narrative that reshapes our understanding of cardioprotection, integrating neuroendocrine, microvascular, and metabolic components into a cohesive framework. It underscores the sophistication of physiological regulation and the potential of targeted molecular interventions in combating cardiovascular disease.
In summary, the discovery that GLP-1 activates K_ATP channels in coronary pericytes, functioning as a critical link in brain-gut-heart communication, represents a major leap in cardiovascular science. It not only elucidates fundamental mechanisms that maintain myocardial perfusion and integrity but also provides fertile ground for innovative therapies aimed at reducing the global burden of heart disease. The convergence of endocrinology, neurobiology, and cardiology embodied in this research exemplifies the future of precision medicine and systemic disease management.
Subject of Research: Investigation of the molecular mechanisms by which GLP-1 activates K_ATP channels in coronary pericytes, mediating brain-gut-heart signaling pathways that promote cardioprotection.
Article Title: GLP-1 activates K_ATP channels in coronary pericytes as the effector of brain-gut-heart signalling mediating cardioprotection.
Article References:
Mastitskaya, S., de Freitas, F.S.S., Evans, L.E. et al. GLP-1 activates KATP channels in coronary pericytes as the effector of brain-gut-heart signalling mediating cardioprotection. Nat Commun (2026). https://doi.org/10.1038/s41467-026-69555-1
Image Credits: AI Generated
Tags: ATP-sensitive potassium channels in heartbrain-gut-heart signalingcoronary microvasculature researchcoronary pericytes functionGLP-1 cardioprotective mechanismsglucagon-like peptide-1 rolesheart disease therapiesinnovative heart disease treatmentsmetabolic integration in cardiovascular healthmyocardial blood flow regulationneuroendocrine and cardiovascular biologyvascular protection in heart