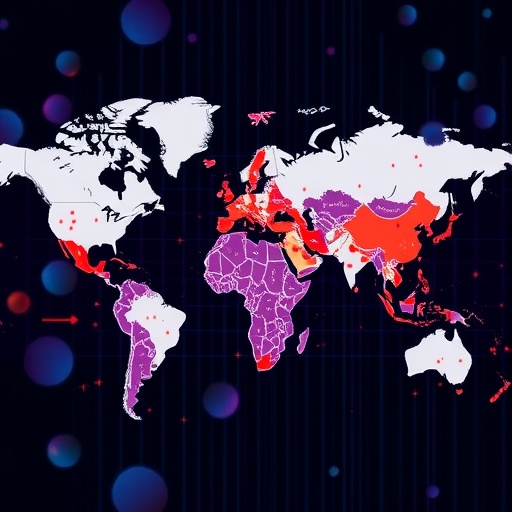
The rise of metabolic-dysfunction-associated steatotic liver disease, type 2 diabetes mellitus, obesity, and cardiovascular disease signifies a pivotal public health crisis recognized globally. The intricate relationship among these conditions has given rise to a concept known as the cardiovascular–liver–metabolic (CLM) syndemic. This term encapsulates the interplay of these diseases, which share common mechanisms and are influenced by socioeconomic factors. They do not exist in isolation; rather, they coexist in a manner that amplifies their individual and collective impacts on public health.
Looking at the statistics, the incidence of CLM diseases is alarming, with millions of individuals impacted worldwide. Each condition exacerbates the severity of the others, creating a vicious cycle of poor health outcomes. The CLM syndemic thus represents a complex network of interactions among risk factors, biological pathways, and environmental influences. This realization necessitates a shift in public health strategies, emphasizing the importance of a multi-faceted approach that addresses these interconnected conditions simultaneously.
At the micro level, enhancing risk prediction and precision prevention strategies emerges as a crucial intervention. By utilizing comprehensive epidemiological data, health professionals can better identify individuals at risk of developing these conditions. This predictive capability can lead to the implementation of targeted interventions, which are essential in curtailing the incidence rates of these diseases. Unique predictors, such as genetic predisposition and lifestyle choices, must be integrated into these predictive models to provide a more accurate risk assessment.
Moving outward to the meso level, the focus shifts to the community and its role in promoting CLM health. Ensuring access to healthy foods and creating environments conducive to physical activity are fundamental. These community-driven initiatives become integral in fostering healthier lifestyles that mitigate the risks associated with the syndemic. Public spaces should be designed to encourage movement, while food systems should prioritize the availability of nutritious options. Collaboration among community stakeholders is essential to cultivate these access points, as they directly influence the health behaviors of individuals.
The macro level introduces a broader perspective on societal determinants that influence health inequities. Addressing systemic factors such as socioeconomic status, education access, and healthcare disparities is paramount in eliminating the barriers to health equity. Advocating for policy changes that promote equitable access to health resources is vital. This broader framework encompasses long-term strategies aimed at dismantling the social injustices that contribute significantly to the prevalence of CLM diseases. Comprehensive public health policies should be enforced to ensure equal opportunities for all individuals to attain and maintain their health.
Moreover, the integration of multi-system intervention strategies presents a promising approach to tackle the trajectories of the CLM syndemic. These strategies must be adaptable and sensitive to the unique needs of diverse populations, recognizing that a one-size-fits-all approach will not suffice. Engagement of various disciplines, including public health, nutrition, epidemiology, and social work, can enhance the effectiveness of these interventions.
Furthermore, the promotion of healthy lifestyle behaviors—such as regular physical activity, balanced nutrition, and mental health support—becomes imperative. Education and awareness campaigns targeted at different demographics can facilitate a culture of health. Knowledge dissemination via community workshops, social media platforms, and public service announcements can empower individuals to make informed choices about their health.
Innovative technology can also play a pivotal role in managing and mitigating the risks associated with CLM diseases. Mobile health applications, wearable devices, and telehealth services could revolutionize patient engagement and enable continuous monitoring of individual health metrics. These technological interventions can provide real-time feedback, motivating individuals to adhere to their prescribed health regimens while fostering accountability.
Research is mandatory to further explore the dynamic interactions between these diseases, focusing on their biological underpinnings and shared pathways. With increasing collaboration across sectors, researchers can work towards uncovering new therapeutic targets and effective interventions. Longitudinal studies that track the evolution of these conditions can yield invaluable insights into modifying risk factors and improving patient outcomes.
As we delve deeper into the ramifications of the CLM syndemic, acknowledging the cultural and societal variables that affect health behaviors is crucial. Community engagement and the integration of cultural competence in public health initiatives can enhance participation and effectiveness. Strategies that resonate with the values and beliefs of target populations can foster a stronger commitment to health improvement efforts.
In conclusion, addressing the cardiovascular–liver–metabolic syndemic requires a paradigm shift in public health approaches. A unified model that employs micro, meso, and macro strategies will not only enhance disease management but also promote overall community well-being. Collaboration among health professionals, policymakers, and the public is essential to develop sustainable solutions that can redirect the current trajectory of these interconnected epidemics into a healthier future for all.
Taking bold steps towards an integrated approach can mend the fabric of public health, intertwining disease prevention with promotion. The journey towards mitigating the impacts of the CLM syndemic hinges on our commitment to collective action, reflecting a true partnership among all stakeholders involved. As the dialogue surrounding CLM diseases evolves, the urgency for actionable solutions becomes more apparent, urging us to rise to the challenge.
Despite the complexity of the CLM syndemic, optimism lies in the potential for innovative solutions. By fortifying community bonds, leveraging technological advancements, and prioritizing health equity, society can create an environment where metabolic health flourishes. This endeavor is not solely about treating illness but rather about fostering a future where individuals thrive—physically, mentally, and socially.
As we look to the horizon, it is clear that the battle against the CLM syndemic is far from over. However, with dedication and a concerted effort, health professionals and communities alike can change the narrative. Now is the time to harness our collective capabilities and transform our approach to health, ultimately paving the way for a healthier generation.
Subject of Research: Cardiovascular–liver–metabolic syndemic epidemiology, trends, and public health challenges.
Article Title: The global cardiovascular–liver–metabolic syndemic: epidemiology, trends and challenges.
Article References:
Chew, N.W.S., Mehta, A., Goh, R. et al. The global cardiovascular–liver–metabolic syndemic: epidemiology, trends and challenges. Nat Rev Cardiol (2025). https://doi.org/10.1038/s41569-025-01220-4
Image Credits: AI Generated
DOI: 10.1038/s41569-025-01220-4
Keywords: Cardiovascular disease, metabolic dysfunction, liver disease, obesity, public health, epidemiology, health equity.
Tags: CLM syndemic complexitiesepidemiological data utilizationglobal cardiovascular disease trendsinterconnected health conditionsliver disease public health crisismetabolic syndrome challengesmulti-faceted public health approachesobesity and cardiovascular healthprecision prevention in healthcarerisk prediction in chronic diseasessocioeconomic factors in healthType 2 diabetes management strategies