In a groundbreaking study published in the World Journal of Pediatrics, researchers have unveiled new insights into the role of cardiac magnetic resonance imaging (CMR) integrated with genetic analysis in the management and prognosis of pediatric heart failure patients suffering from nonischemic etiologies. Pediatric heart failure remains a complex and multifaceted syndrome, often leading to significant morbidity and mortality in affected children. The study spearheaded by Gao, Chen, and Bo et al., pushes the boundaries of conventional diagnostic paradigms, shedding light on how advanced imaging technologies combined with molecular genetics can revolutionize the understanding of disease progression and therapeutic strategies in this vulnerable population.
Heart failure in children, particularly when nonischemic in origin, presents unique diagnostic challenges. Unlike ischemic heart disease commonly seen in adults, pediatric nonischemic heart failure encompasses a spectrum of underlying pathologies including cardiomyopathies, myocarditis, and genetic cardiogenetic disorders. These conditions often exhibit heterogeneous clinical presentations and variable outcomes, complicating clinical decision-making. The current study leveraged state-of-the-art CMR techniques to delineate myocardial tissue characteristics with precision, capturing nuances invisible to conventional echocardiography or standard clinical evaluation.
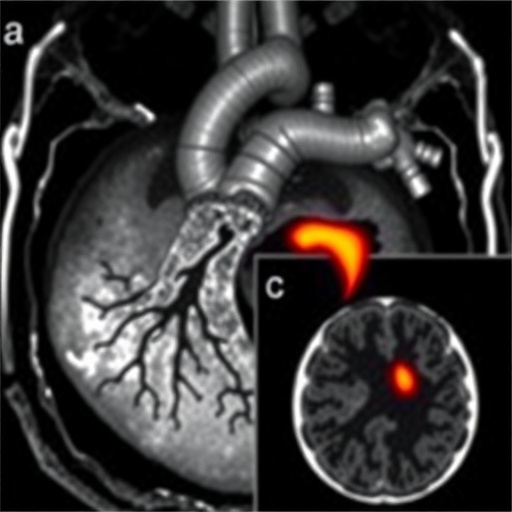
At the heart of the research lies the integration of detailed phenotypic data from CMR with comprehensive genetic screening, focusing on pathogenic variants predisposing to cardiac dysfunction. This dual-pronged approach not only enhances diagnostic accuracy but also facilitates prognostic stratification, enabling clinicians to identify children at heightened risk of adverse outcomes. The researchers utilized advanced myocardial mapping sequences, including late gadolinium enhancement (LGE) and T1/T2 mapping, to visualize myocardial fibrosis, edema, and inflammation repeatedly implicated in disease mechanisms underlying nonischemic heart failure.
.adsslot_GIAsRrK6lW{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_GIAsRrK6lW{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_GIAsRrK6lW{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Beyond structural imaging, the genetic component of the study deployed next-generation sequencing to uncover cryptic mutations within well-known cardiomyopathy-associated genes as well as novel loci potentially contributing to disease phenotypes. The confluence of such genetic markers with imaging biomarkers allowed the team to correlate genotype-phenotype relationships with clinical trajectories, unveiling subgroups of patients that might benefit from tailored therapeutic interventions, including novel pharmacological agents or early consideration for mechanical circulatory support.
Significantly, the study’s longitudinal design permitted analysis of the prognostic value of combined CMR and genetic data over follow-up periods extending beyond two years. The predictive models developed demonstrated superior sensitivity and specificity in anticipating adverse cardiac events, such as sudden cardiac death, hospitalizations for decompensated heart failure, or need for transplantation. This represents a vital advance, as early identification of high-risk pediatric patients can prompt timely escalation of care and personalized management plans.
Moreover, the findings implicate the presence and extent of myocardial fibrosis detected by LGE as a critical determinant of prognosis. Fibrotic tissue not only serves as a substrate for arrhythmogenesis but also reflects ongoing pathological remodeling processes unaddressed by standard heart failure therapies. The study highlighted how fibrosis burden quantified through CMR correlated with deleterious outcomes, underscoring the need to incorporate imaging biomarkers into routine clinical surveillance.
Importantly, the research team emphasized the importance of genetics in distinguishing phenocopies and overlapping cardiomyopathy syndromes, which often confound clinical interpretation. Genetic testing emerged as indispensable for elucidating underlying molecular drivers, enabling stratification of patients into genetically defined subtypes with distinct natural histories. For example, mutations in sarcomeric protein genes versus desmosomal protein alterations appeared to confer differing risk profiles, influencing prognosis and therapeutic responsiveness.
The investigators also stressed the evolving role of CMR tissue characterization techniques in detecting subtle myocardial changes indicative of disease activity, such as inflammation and edema, which may precede overt functional deterioration. Such insights pave the way for early intervention aimed at halting or reversing pathological remodeling before irreversible damage ensues. This proactive approach aligns with the precision medicine paradigm, integrating molecular and imaging data for optimized pediatric heart failure care.
One of the study’s remarkable contributions is its demonstration that the marriage of genetic data with CMR metrics yields additive prognostic information beyond either modality alone. This integrative model offers a holistic view of the disease state by combining structural, functional, and molecular data, a framework that might be extended to other complex cardiac conditions in pediatrics and adults alike. The approach augurs a future where diagnosis and prognosis are no longer confined to clinical symptoms and echocardiography but are refined by multifaceted, high-resolution assessments.
While the study traversed new frontiers, it also acknowledged certain limitations, including the challenges in interpreting variants of uncertain significance and the need for broader genetic panels to capture the full spectrum of pathogenic mutations. Likewise, uniform access to CMR remains constrained in many regions, calling for strategies to democratize these advanced diagnostics to achieve equitable pediatric cardiac care.
Clinically, the implications of this research are multifarious. Enhanced risk stratification can inform individualized surveillance intervals, medication regimens, and decisions regarding implantable defibrillators or transplantation candidacy. For families and caregivers, understanding genetic underpinnings provides clarity on prognosis and informs genetic counseling and screening of at-risk relatives, thereby extending benefits beyond the index patient.
Furthermore, the study stimulates avenues for research into targeted therapies aimed at molecular pathways implicated by genetic findings, as well as novel anti-fibrotic agents guided by imaging biomarkers. It also lays the groundwork for integrating artificial intelligence algorithms to analyze complex imaging-genomic datasets, potentially accelerating discovery and clinical translation.
In sum, the comprehensive evaluation presented by Gao and colleagues represents a paradigm shift in the pediatric heart failure domain. By harnessing the power of cardiac magnetic resonance imaging alongside genomic analysis, the study elevates the precision of diagnosis, prognosis, and management in nonischemic pediatric heart failure. As technology continues to evolve, such integrative strategies herald a new era where individualized medicine can transform outcomes for children grappling with this formidable cardiovascular condition.
The future of pediatric cardiology appears poised for a transformation driven by multidisciplinary collaborations bridging imaging science, molecular genetics, and clinical cardiology. Studies like this not only deepen scientific understanding but also bear profound implications for improving quality of life and survival rates among affected children globally. The challenges of implementation notwithstanding, the promise of such integrated diagnostics is undeniable, paving the way for personalized, effective, and timely therapeutic interventions.
Officials and clinicians are already taking note of these findings, recognizing the potential to refine guidelines and protocols related to pediatric heart failure evaluation. Importantly, these advancements may stimulate policy changes advocating for wider availability of advanced cardiac imaging and genetic testing in pediatric patients suspected of heart failure, particularly in the nonischemic subset often underserved by existing diagnostic criteria.
Given the complexity of heart failure in children, multidisciplinary teams involving pediatric cardiologists, geneticists, radiologists, and specialized nurses will be vital in translating these research insights into clinical practice. Collaborative efforts will ensure that children receive comprehensive care shaped by the latest evidence, improving prognosis and minimizing complications associated with delayed or inaccurate diagnosis.
Moreover, this landmark study underscores the importance of patient registries and databases incorporating detailed imaging and genetic data to facilitate ongoing research and refinement of prognostic models. The future will likely see expansion of such datasets internationally, enabling meta-analyses and cross-population studies that can uncover novel genotype-phenotype correlations and regional variations, tailoring interventions to diverse patient groups.
Overall, the integration of cardiac magnetic resonance imaging and genetic profiling in pediatric nonischemic heart failure promises to rewrite the narrative of this challenging clinical entity. It invites a new era of deeper, more nuanced understanding that transcends traditional diagnostic silos, ultimately reshaping care paradigms and offering hope to countless children and families affected by heart failure worldwide.
Subject of Research: Cardiac magnetic resonance imaging combined with genetic analysis for prognosis in pediatric nonischemic heart failure
Article Title: Cardiac magnetic resonance and genetics in pediatric heart failure patients with nonischemia: prognostic implications
Article References:
Gao, XL., Chen, Y., Bo, KR. et al. Cardiac magnetic resonance and genetics in pediatric heart failure patients with nonischemia: prognostic implications. World J Pediatr 21, 489–501 (2025). https://doi.org/10.1007/s12519-025-00920-8
Image Credits: AI Generated
DOI: May 2025
Tags: advanced imaging technologies in medicinecardiac MRI in childrenclinical decision-making in pediatricsdisease progression in heart failuregenetic analysis in cardiologyinnovative diagnostic techniquesmolecular genetics and heart diseasemyocarditis in childrennonischemic heart failure causespediatric cardiomyopathies researchpediatric heart failure managementtherapeutic strategies for pediatric heart conditions