In an enlightening study that spans across critical pediatric care, researchers have unveiled significant findings concerning fluid management in critically ill children. The paper, authored by Utami et al., discusses the intricate relationship between positive fluid balances and specific ultrasound scores in cases of fluid overload—a situation all too common in pediatric intensive care units. Fluid overload in critically ill children can lead to a plethora of complications, including respiratory distress and cardiovascular instability. Consequently, understanding the nuances of fluid balance becomes paramount in the course of treatment.
The investigation delves into the correlation between positive fluid balances and venous excess, assessed through advanced ultrasound techniques. The study’s authors emphasize that maintaining a precise fluid balance is essential, as both excess and deficit can have dire consequences for pediatric patients. By employing venous excess ultrasound scores, healthcare professionals gain insight into the patient’s fluid status, enabling more targeted and effective interventions.
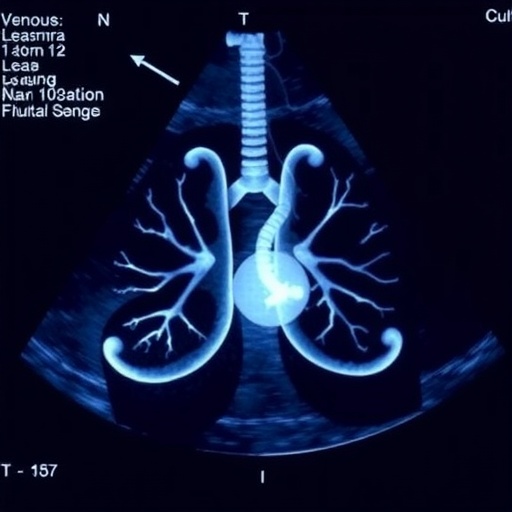
Lung ultrasound, another key component of the study, offers a non-invasive method to evaluate pulmonary congestion and fluid overload, a crucial aspect considering that the respiratory system is often the first to be compromised in such patients. The authors provide a compelling argument that combining venous excess ultrasound scores with lung ultrasound findings could revolutionize how clinicians assess fluid overload in critically ill children.
Drawing from a well-defined cohort, the authors meticulously analyzed the data, substantiating their observations with robust statistical analysis. Their findings illuminate how an accurate assessment of fluid status can lead to improved clinical outcomes. This study not only contributes to the existing body of literature but also paves the way for future research in pediatric fluid management.
In the realm of critical care, where every decision can have life-altering consequences, the implementation of advanced ultrasound techniques can prove invaluable. The authors advocate for a paradigm shift that prioritizes tailored fluid management strategies, derived from the real-time insights provided by ultrasound assessments. The interplay between venous excess and lung ultrasound measurements may offer a comprehensive picture of a child’s fluid status, leading to better-informed clinical decisions.
Furthermore, the implications of this research extend beyond immediate clinical settings. The study underscores the importance of continuous education and training for healthcare professionals in utilizing these innovative ultrasound technologies effectively. As the landscape of pediatric critical care continues to evolve, embracing such advancements will ensure that practitioners can offer the highest standard of care to their most vulnerable patients.
As hospitals worldwide grapple with the challenge of managing fluid overload, the findings from Utami et al. serve as a vital resource. Critically ill children are often unable to express their discomfort, making it imperative for caregivers to rely on objective measures to guide their treatment. The nuanced understanding of how positive fluid balances correlate with sonographic findings equips clinicians with the tools necessary to navigate these complex cases confidently.
Moreover, the ethical considerations surrounding fluid management cannot be overlooked. The findings of the study stress that indiscriminate fluid administration can lead to unwarranted adverse effects. Therefore, it is the responsibility of healthcare providers to critically evaluate each patient’s fluid requirements based on the evidence presented in the study. This approach not only enhances patient safety but also optimizes the use of medical resources.
Looking ahead, the researchers call for larger, multicentric studies to augment the validity of their findings. They envision a future where rigorous protocols based on their research integrate seamlessly into daily clinical practice. With the ongoing evolution of medical technology, the potential for further advancements in ultrasound techniques may yield even more precise assessments of fluid overload in pediatric populations.
The implications of this study also resonate with the broader field of pediatric medicine, where fluid management has long been a contentious issue. By advocating for a more refined approach to assessing fluid status through ultrasound, Utami et al. may influence pediatric protocols beyond critical care, affecting general hospital practices and outpatient management of childhood illnesses.
In conclusion, the research presented by Utami and colleagues represents a significant step forward in understanding fluid management in critically ill children. The correlation between positive fluid balances and ultrasound scores opens new avenues for improving patient outcomes in the challenging environment of pediatric intensive care. As we continue to seek advancements in medical practice, studies like this provide the essential foundation needed to foster innovation and improve care for our youngest and most vulnerable patients.
While the study itself is a tremendous addition to the literature, it also raises follow-up questions regarding individual variability in fluid management. Can pediatric patients with specific comorbidities benefit differently from the insights provided by ultrasound assessments? Future research may delve into these specifics, tailoring approaches that consider the unique physiological responses of each child.
Ultimately, it is the proactive and data-driven strategies that will define the future of pediatric critical care. The synergy of clinical expertise and cutting-edge technology, as demonstrated in this research, will empower healthcare providers to make timely and effective decisions that enhance recovery and patient safety.
Subject of Research: Correlation between fluid balances and ultrasound assessments in critically ill children with fluid overload.
Article Title: Correlation between positive fluid balances with venous excess ultrasound scores and lung ultrasound in critically ill children with fluid overload.
Article References:
Utami, M.D., Prawira, Y., Djer, M.M. et al. Correlation between positive fluid balances with venous excess ultrasound scores and lung ultrasound in critically ill children with fluid overload. BMC Pediatr 25, 858 (2025). https://doi.org/10.1186/s12887-025-06177-4
Image Credits: AI Generated
DOI: 10.1186/s12887-025-06177-4
Keywords: fluid overload, pediatric intensive care, venous excess ultrasound scores, lung ultrasound, fluid management.
Tags: cardiovascular instability in childrencomplications of fluid overload in childrencorrelation between fluid overload and ultrasound scoresfluid balance management in pediatric carelung ultrasound for fluid overloadnon-invasive ultrasound techniquespediatric fluid management strategiespediatric intensive care unit challengespositive fluid balance implicationsrespiratory distress and fluid overloadtargeted interventions for fluid managementvenous ultrasound in critically ill children