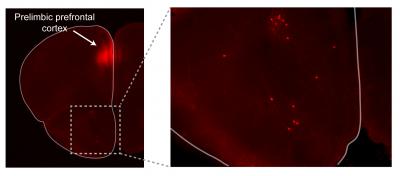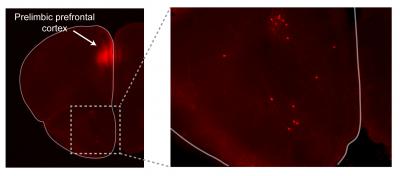
Credit: Andrew Moberly, Perelman School of Medicine, University of Pennsylvania
PHILADELPHIA – "Take a deep breath" is the mantra of every anxiety-reducing advice list ever written. And for good reason. There's increasing physiological evidence connecting breathing patterns with the brain regions that control mood and emotion.
Now, Minghong Ma, PhD, a professor of Neuroscience in the Perelman School of Medicine at the University of Pennsylvania, and Penn doctoral student Andrew Moberly, have added neurons associated with the olfactory system to the connection between behavior and breathing. These findings are published this week in Nature Communications. Connecting patterns in these interactions may help explain why practices such as meditation and yoga that rely on rhythmic breathing can help people overcome anxiety-based illnesses.
"We wanted to know why and how fear behavior, controlled breathing, and smell centers of the brain were connected," Ma said. "What really drives our interest is finding out what we can extrapolate about this relationship to learn about the evolution of behavior and apply this knowledge to help ease the pain associated with such disorders as post-traumatic stress disorder."
In earlier studies, Ma found that ends of neurons in the nose have odor sensors as well as the ability to detect the rate of breathing. "The nose really does double duty in its function," Moberly said. "Why and what role does this have in behavior and what does that fear behavior look like in rodents? Their behavioral choices for survival are fight, flight, or freeze."
To tease apart these overlapping characteristics, Moberly first trained mice by pairing a specific sound with a light foot shock to induce "freezing" in the normally mobile mice. Freezing behavior is a quiescent period that is unusual for scurrying mice. When he plays the sound associated with the foot shock, "trained" mice literally freeze in their tracks.
Other groups have observed that the amygdala and prelimbic prefrontal cortex, which govern learning and memory, emotion, and decision-making, were electrically active during "freezing," at an average of 4 Hz. Moberly observed that freeze behavior, breathing rate, and electrical activity of these brain regions were coordinated literally on the same wavelength.
Knowing that humans have the ability to voluntarily control the breathing patterns, "now the field is asking, how do we breathe differently in different emotional situations," Ma said. "Evolutionarily this makes sense. If a mouse in the wild senses danger by smell, for example, it may freeze and slow down breathing as a survival instinct. Now we want to know how we can apply that knowledge to humans. It would be interesting to find out what breathing patterns are most effective in influencing human brain activity and emotional states"
###
Other coauthors include Mary Schreck, Janardhan Bhattarai, and Wenqin Luo, all from Penn, and Larry S. Zweifel from the University of Washington.
This work was supported by grants from the National Institute of Deafness and Other Communication Disorders (R01DC006213) and the National Science Foundation (1515930).
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $7.8 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $405 million awarded in the 2017 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center — which are recognized as one of the nation's top "Honor Roll" hospitals by U.S. News & World Report — Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; Penn Wissahickon Hospice; and Pennsylvania Hospital – the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine, and Princeton House Behavioral Health, a leading provider of highly skilled and compassionate behavioral healthcare.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2017, Penn Medicine provided $500 million to benefit our community.
Media Contact
Karen Kreeger
[email protected]
215-459-0544
@PennMedNews
http://www.uphs.upenn.edu/news/