Obstructive Sleep Apnea (OSA) and Metabolic Syndrome (MetS) are two increasingly prevalent health conditions that pose significant risks to cardiovascular health. The interconnectedness of these disorders creates a complex web that affects millions globally. Both conditions have been documented as having a serious impact on various physiological processes, ultimately leading to increased morbidity and mortality. The intricate relationship between OSA, MetS, and obesity is gaining attention in the medical community, with mounting evidence indicating that these disorders not only coexist but also exacerbate each other in a cyclical pattern.
OSA is characterized by recurrent episodes of airway obstruction during sleep, leading to intermittent hypoxia and disrupted sleep patterns. It affects an estimated 14% of the global population, particularly among individuals aged 30 to 69. Typically, those suffering from OSA experience notable symptoms such as loud snoring, excessive daytime sleepiness, fatigue, and morning headaches. Its prevalence increases dramatically with body weight, indicating a straightforward link to obesity. Individuals grappling with OSA are often caught in a vicious cycle wherein their sleep disordered breathing contributes to weight gain, thereby worsening their OSA symptoms.
On the other hand, MetS consists of a cluster of metabolic abnormalities including central obesity, hypertension, dyslipidemia, insulin resistance, and elevated blood sugars. The National Cholesterol Education Program estimates that approximately 24% of the U.S. population currently suffers from MetS. The overlapping risk factors of OSA and MetS result in a notable increase in prevalence, intensifying the health risks associated with them. With such alarming statistics, it becomes evident that understanding the bidirectional relationship between OSA and MetS is crucial for healthcare professionals.
Scientific research underscores the interrelation between OSA and MetS, particularly emphasizing how severity levels of one condition can influence the prevalence of the other. Studies demonstrate a significant rise in MetS occurrences correlating directly with the severity of OSA, with rates climbing as high as 57.1% in patients with severe forms of the condition. Conversely, the presence of MetS significantly increases the likelihood of individuals developing OSA, presenting a quintessential chicken-and-egg scenario. This relationship poses unique challenges in treating either condition effectively.
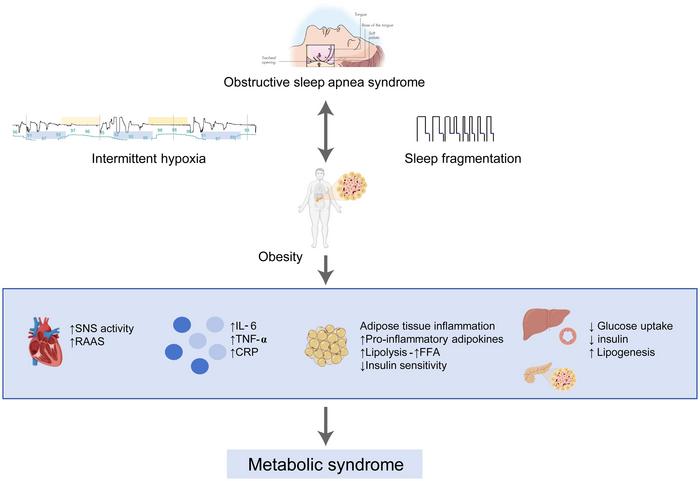
Crucially, obesity acts as a mediator in the relationship between OSA and MetS. Increased visceral fat leads to enhanced airway collapse and escalating inflammation, exacerbating OSA symptoms. Likewise, chronic intermittent hypoxia—a hallmark of OSA—triggers metabolic disruptions, potentially resulting in the onset of MetS. Thus, addressing obesity becomes vital in disentangling the web binding these disorders, laying the groundwork for effective interventions.
The pathophysiological mechanisms connecting OSA and obesity are ingrained in hormonal dysregulation. Increasing evidence indicates that every 10% rise in body weight can lead to a 32% increase in the apnea-hypopnea index (AHI), which is a benchmark measure of OSA severity. This relationship highlights the need for targeted weight management strategies in individuals with OSA. Additionally, hormonal issues such as leptin resistance and increased ghrelin levels further complicate weight management, leading to heightened appetite and subsequent weight gain among OSA patients.
Hypertension has also been garnering attention in discussions surrounding OSA and MetS. Research indicates that there is a strong correlation between OSA and hypertension, elucidated by findings from the Wisconsin Sleep Cohort study. Notably, individuals suffering from severe OSA face three times the likelihood of developing hypertension as those without sleep-disordered breathing. This relationship can be traced back to the disruption of normal blood pressure regulation due to sympathetic nervous system overactivity, exacerbated by chronic intermittent hypoxia and sleep fragmentation.
Furthermore, the relationship between OSA and diabetes has emerged as a focus of many studies. As sleep quality deteriorates due to OSA, insulin resistance increases, leading to greater risks of developing type 2 diabetes mellitus. Conditions precipitated by sleep fragmentation and hypoxia have been linked to impaired glucose metabolism, increased sympathetic activity, and elevated inflammatory cytokines. Consequently, patients with OSA display elevated fasting glucose levels and often grapple with uncontrolled blood sugar.
The connection between OSA and dyslipidemia cannot be overlooked as well. Dyslipidemia is a characteristic component of MetS, frequently occurring alongside OSA. Severe cases of OSA are associated with low levels of high-density lipoprotein (HDL) and elevated concentrations of triglycerides and low-density lipoprotein (LDL). The alterations in lipid metabolism caused by chronic intermittent hypoxia underscore the vital role of lipid management in patients with OSA, as these disruptions can lead to extensive cardiovascular complications.
Lifestyle changes represent a cornerstone of treatment, focusing on dietary modifications and physical activity as foundational components in managing MetS. Significant weight loss has been shown to lead to improvements in both OSA severity and metabolic health parameters, emphasizing the importance of comprehensive lifestyle interventions. An integrated approach that combines CPAP therapy with lifestyle changes can significantly improve overall health outcomes for patients.
In certain cases, metabolic surgeries, such as gastric bypass or sleeve gastrectomy, present options for obese patients suffering from both OSA and MetS. These procedures promote long-term weight loss and drive meaningful improvements in insulin resistance and hypertension. Emerging data suggest that metabolic surgical options can lead to sustained relief from OSA symptoms and reduce reliance on CPAP devices, showcasing their potential as an impactful treatment modality.
Looking towards the future, the increasing focus on precision medicine aimed at tailoring treatment to the individual is particularly promising. By investigating the molecular underpinnings of chronic intermittent hypoxia and its metabolic consequences, researchers aim to identify novel therapeutic targets to break the interdependence of OSA and MetS. Longitudinal studies will play a critical role in evaluating the impact of integrated treatment approaches on patient health outcomes, reinforcing the need to address both conditions concurrently.
As we continue to delve deeper into understanding the complex relationship between obstructive sleep apnea and metabolic syndrome, it becomes increasingly evident that a concentrated, multi-disciplinary approach is essential. Breaking the cycle that binds these conditions together isn’t just a health imperative; it is crucial for reducing cardiovascular risks and improving patient quality of life. As more research unfolds, the path towards effective treatment is beginning to take shape, illuminating a clearer horizon for those affected by these intertwined disorders.
Subject of Research: The complex relationship between Obstructive Sleep Apnea and Metabolic Syndrome
Article Title: The Interconnected Nature of Obstructive Sleep Apnea, Obesity, and Metabolic Syndrome
News Publication Date: [Insert Current Date]
Web References: [Insert relevant links]
References: [Insert relevant academic references]
Image Credits: [Insert relevant credit for any images]
Keywords: Obstructive Sleep Apnea, Metabolic Syndrome, Obesity, Cardiovascular Health, Insulin Resistance, Hypertension, Dyslipidemia, CPAP Therapy, Lifestyle Modifications, Metabolic Surgery.
Tags: cardiovascular risks of OSAchronic health issues and sleep apneacyclical pattern of OSA and obesitydaytime sleepiness and health consequencesinterconnected health conditionsmanaging sleep disorders and weight loss.metabolic abnormalities in MetSMetabolic Syndrome and obesity relationshipobesity impact on sleep qualityObstructive Sleep Apnea treatment advancespathophysiology of sleep disorderssleep apnea prevalence statistics