Genital tuberculosis, a formidable yet often overlooked form of extrapulmonary tuberculosis, poses significant challenges in terms of diagnosis, treatment, and implications for reproductive health. This pervasive infection is primarily caused by Mycobacterium tuberculosis and can lead to devastating consequences for women’s reproductive systems. The comprehensively reviewed patterns of this disease underscore the need for heightened awareness and improved diagnostic strategies among healthcare professionals and the public alike. Scholars have delved deep into the intricacies of genital tuberculosis, revealing complex patterns that demand attention in the medical community.
The epidemiological data surrounding genital tuberculosis paints a sobering picture. This condition is not limited to developing nations but can also surface in more economically developed regions, albeit often underdiagnosed due to its non-specific symptoms. Factors such as socioeconomic status, cultural practices, and healthcare access play critical roles in the prevalence of genital tuberculosis. The rising rates of infection in populations, particularly in certain demographic groups, necessitate a reevaluation of public health strategies to address this public health concern effectively.
One of the key findings in the current literature is that genital tuberculosis is often asymptomatic in its early stages, which complicates early diagnosis. Women may experience subtle changes in menstrual patterns or mild pelvic pain, which can easily be dismissed. As the disease progresses, however, more severe symptoms can manifest, including profound pain during intercourse, infertility, and abnormal vaginal discharge. These symptoms often lead women to seek medical advice only when the infection has reached an advanced stage, thereby complicating treatment outcomes and raising concerns about the long-term effects on fertility.
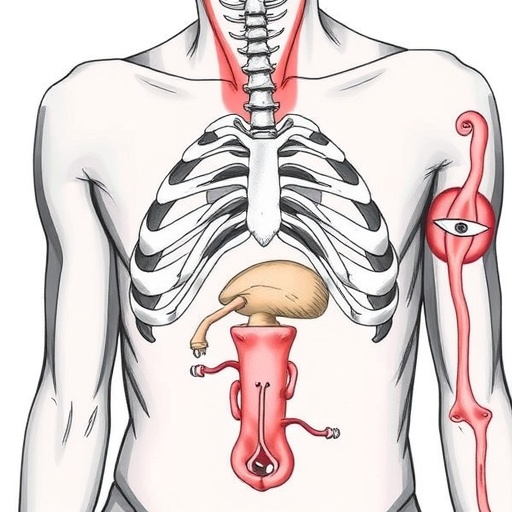
The pathophysiology of genital tuberculosis involves the spread of the Mycobacterium tuberculosis bacteria from the lungs or other body parts to the reproductive system. This can occur through different mechanisms, including lymphatic spread. The infection can affect various reproductive organs, including the ovaries, fallopian tubes, and uterus, causing lesions that can lead to scarring and obstruction. These physiological changes considerably hinder fertility and can result in ectopic pregnancies, highlighting the need for awareness and prompt intervention.
Diagnostic strategies for genital tuberculosis have significantly evolved over the years. Traditional methods, such as pelvic examinations and culture tests, can be time-consuming and may lack sensitivity. Modern modalities like polymerase chain reaction (PCR) testing have entered the realm of clinical practice, providing rapid and accurate diagnoses. Additionally, imaging techniques such as transvaginal ultrasound and magnetic resonance imaging (MRI) are becoming indispensable tools in identifying complications associated with genital tuberculosis, ensuring better management of the condition.
Despite advancements in diagnostics and awareness, therapeutic approaches to treating genital tuberculosis remain a challenge. The standard treatment protocol typically involves a multi-drug regimen that may last several months. However, adherence to treatment can be problematic due to side effects and the lengthy duration required for effective resolution of the infection. Physicians must not only focus on eradicating the bacteria but also on managing the patient’s overall health and addressing complications that may affect fertility during and after the treatment period.
Emerging research continues to highlight the psychosocial impacts of genital tuberculosis on affected women, often overlooked in traditional medical literature. The stigma associated with tuberculosis, compounded by its implications for fertility, can lead to feelings of isolation and despair. Women may experience anxiety about their reproductive potential, which can significantly affect their mental health. It is essential for healthcare providers to adopt a holistic approach, considering both the physical and emotional well-being of patients as part of comprehensive care.
Further complicating the landscape is the co-infection of tuberculosis with other sexually transmitted infections (STIs). Having concurrent STIs can exacerbate the severity of genital tuberculosis and complicate diagnoses and treatment. Therefore, employing a multi-faceted approach involving screening for other infections has become increasingly vital in managing patients. This integrative strategy not only enhances patient outcomes but also aids in reducing transmission rates within communities.
Public health initiatives aimed at raising awareness about genital tuberculosis are crucial to curbing its spread. Educational programs highlighting the risks, symptoms, and need for regular gynecological check-ups can empower women and the general public to seek timely medical intervention. Such awareness campaigns must also focus on reducing the stigma surrounding tuberculosis, promoting understanding that it is a treatable condition with adequate medical care and support.
In light of these insights, professionals in reproductive health and infectious disease must collaborate closely to address both the medical and social dimensions of genital tuberculosis. This necessitates advocacy for increased funding for research, enhanced training for healthcare professionals, and community outreach programs aimed at educating populations at risk. Such coordinated efforts can potentially reshape the landscape of genital tuberculosis, transforming it from a chronic public health issue into a manageable condition.
In conclusion, genital tuberculosis remains a pressing concern that transcends geographic and socioeconomic boundaries. Continued research into its pathophysiology, diagnostics, and socio-psychological implications is imperative. As the body of knowledge about this condition grows, there’s hope for improved outcomes for women afflicted with this ailment, fostered by early diagnosis and comprehensive, compassionate care that takes into account the delicate interplay of physical and emotional health.
As we advance our understanding of genital tuberculosis through ongoing research, it becomes increasingly evident that a multifaceted approach is vital for tackling this complex disease. Awareness, early diagnosis, effective treatment, and patient-centered care are the cornerstones of overcoming the challenges posed by genital tuberculosis, ultimately leading to better fertility outcomes and overall life quality for affected women.
Subject of Research: Genital Tuberculosis
Article Title: Comprehensive Review of Genital Tuberculosis: Epidemiological Patterns, Causal Agents, Diagnostic Strategies, Symptomatology and Fertility Consequences
Article References:
Kaur, R., Sharma, V. & Kumari, A. Comprehensive Review of Genital Tuberculosis: Epidemiological Patterns, Causal Agents, Diagnostic Strategies, Symptomatology and Fertility Consequences.
Reprod. Sci. (2025). https://doi.org/10.1007/s43032-025-01987-4
Image Credits: AI Generated
DOI: [Provide DOI if applicable]
Keywords: Genital Tuberculosis, Mycobacterium tuberculosis, Epidemiology, Fertility, Diagnostics, Public Health, Women’s Health
Tags: asymptomatic genital tuberculosiscultural practices and tuberculosisdiagnosis of genital tuberculosiseffects of genital tuberculosis on reproductive healthepidemiology of genital tuberculosisgenital tuberculosis causesimproving awareness of genital tuberculosisMycobacterium tuberculosis infectionpublic health strategies for tuberculosisreproductive health implications of tuberculosissocioeconomic factors in tuberculosis prevalenceunderdiagnosis of genital tuberculosis