Credit: Venu Raman
An experimental drug that targets abnormally high levels of a protein linked to cancer growth appears to significantly reduce the proliferation of prostate cancer cells in laboratory cell cultures and animals, while also making these cells considerably more vulnerable to radiation, according to results of a study led by Johns Hopkins scientists.
The findings, published Sept. 12 in Cancer Research, could advance the search for novel combination treatments that make more effective and safer use of radiation against prostate cancer, the most common nonskin cancer in men and the second leading cause of cancer-related deaths in men in the United States.
Of the nearly 200,000 men diagnosed with prostate cancer each year in the United States, radiation is a first-line therapy considered for all but the most advanced disease. However, some of these cancers become resistant to the effects of radiation over time, according to Venu Raman, Ph.D., an associate professor of radiology and radiological science and of oncology at the Johns Hopkins University School of Medicine and member of the Johns Hopkins Kimmel Cancer Center.
In a search for ways of extending the value of radiation and limiting the collateral damage to healthy tissue that necessarily high doses of radiation may inflict, Raman worked with Phuoc Tran, M.D., Ph.D., an associate professor of radiation oncology and molecular radiation sciences, oncology, and urology, and also a member of the Kimmel Cancer Center.
They and colleagues from Johns Hopkins and University Medical Centre Utrecht had earlier discovered that a protein called DDX3 appears to be "dysregulated" in many cancers, including breast, lung, colorectal, sarcoma and prostate. The researchers found that the more aggressive the cancer, the higher the expression of this protein, which helps maintain cellular stability.
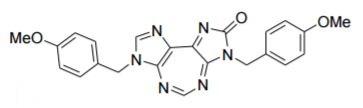
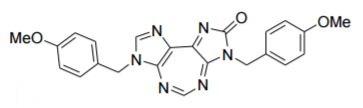
The researchers then developed a molecule referred to as RK-33 that was designed to disrupt DDX3's function by locking on to a portion of the protein. They showed in previous studies with cell cultures that when adding RK-33 to malignant lung and other cancerous cells that highly express DDX3, proliferation slowed or halted, and the cells' ability to form colonies was impaired. Additionally, RK-33 appeared to be a radiosensitizer, making the destructive effects of radiation more pronounced.
In the new study, the researchers began by examining prostate cancer tissue samples from University Medical Centre Utrecht. Of the 23 samples with a Gleason score greater than seven, eight had high DDX3 expression.
As with results of their earlier studies, the investigators found that the higher the expression of this protein, the more aggressive the cancer, which is determined by how the cells invade other tissue types and their ability to form tumors in laboratory models of cancers. When the researchers used gene engineering techniques to knock out DDX3 expression in laboratory-grown cell cultures that highly expressed this protein, cell proliferation was half that of cell cultures with high DDX3 expression.
Incubating cultured cells with RK-33 had a similar effect, knocking down DDX3 expression in cells that highly express this protein and hampering their ability to multiply. When researchers combined the drug with radiation, the effects were synergistic, they report, killing from two to four times more cells than radiation alone.
Next, the researchers tested the effects of RK-33 and radiation in mice that had been injected with human prostate cancer cells that highly express DDX3. The animals formed tumors within a few weeks. Together, Raman says, this dual-mode treatment produced cell-killing results that paralleled their experiments in cell cultures.
Raman adds that the experimental drug appeared to have no toxicity in the mice, suggesting that it could be a promising drug to test in humans. Compounds based on RK-33, he says, might have value in treating a broad array of cancers that highly express DDX33 or as a supplement to radiation, making conventional doses more effective or improving the killing ability of lower doses.
"A lot of work still needs to be done to develop this into a chemotherapy drug," Raman cautions. "But based on our findings, we think it could fill an unmet need in making the most common treatment for prostate cancer more effective."
###
Other Johns Hopkins researchers who participated in this study include Min Xie, Farhad Vesuna, Saritha Tantravedi, Guus M. Bol, Marise R. Heerma van Voss, Katriana Nugent, Reem Malek and Kathleen Gabrielson.
Media Contact
Vanessa Wasta
[email protected]
410-614-2916
@HopkinsMedicine
http://www.hopkinsmedicine.org