In a groundbreaking study unveiled recently, researchers have illuminated the complex metabolic dependencies underpinning triple-negative breast cancer (TNBC), highlighting a nuanced relationship between exogenous cystine uptake and glutamine addiction within malignant cells. This emerging insight not only deepens our comprehension of TNBC’s aggressive nature but also charts new avenues for targeted metabolic interventions, potentially revolutionizing therapeutic strategies for one of the most challenging breast cancer subtypes.
Triple-negative breast cancer is notoriously difficult to treat due to its lack of estrogen receptor, progesterone receptor, and HER2 expression. This absence renders conventional hormonal therapies ineffective, necessitating the search for alternative vulnerabilities intrinsic to TNBC cells. Central to this pursuit is investigating metabolic dependencies that cancer cells exploit to sustain their rapid proliferation and survival under the hostile conditions of a tumor microenvironment.
Metabolic reprogramming is now recognized as a hallmark of cancer, with tumor cells altering nutrient uptake and utilization to meet heightened energetic and biosynthetic demands. Particularly, amino acid metabolism has garnered significant attention, as many cancers exhibit auxotrophies or dependencies on non-essential amino acids produced or acquired from their surroundings. In this recent research, the interplay between cystine, an oxidized dimer of cysteine, and glutamine—a pivotal nitrogen and carbon source for proliferative cells—has been meticulously dissected.
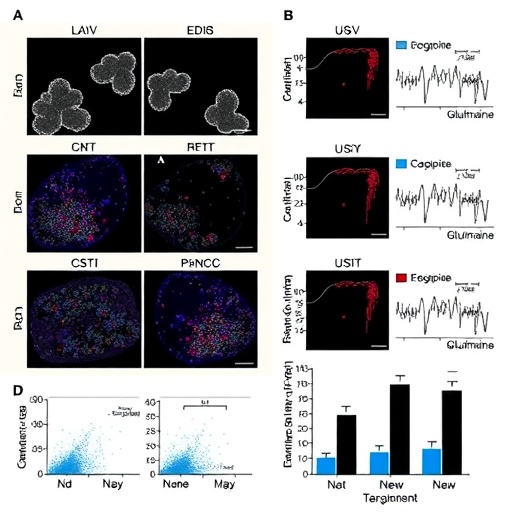
The investigative team employed advanced metabolomics and isotope tracing techniques to monitor how exogenous cystine uptake influences glutamine metabolism within TNBC cells. Findings revealed that cystine availability modulates glutamine dependency by reshaping intracellular redox homeostasis and altering the flow through key metabolic pathways such as the tricarboxylic acid (TCA) cycle and glutaminolysis. This metabolic crosstalk underscores a delicate balance TNBC cells maintain to optimize survival and proliferation.
At the heart of this metabolic interplay lies the cystine/glutamate antiporter system Xc⁻, which facilitates the exchange of extracellular cystine for intracellular glutamate. Elevated activity of system Xc⁻ not only supplies cystine but also depletes intracellular glutamate, directly impacting glutamine catabolism. The researchers demonstrated that increased cystine import via this antiporter triggers compensatory enhancements in glutamine uptake and metabolism, positioning glutamine as a crucial auxiliary substrate for replenishing intracellular glutamate pools and sustaining redox balance.
Redox regulation is critical for cancer cell survival, as reactive oxygen species (ROS) levels fluctuate during rapid proliferation and environmental stress. Cystine-derived cysteine is a precursor for glutathione synthesis, the primary cellular antioxidant. By bolstering glutathione production, TNBC cells safeguard themselves against oxidative damage. This metabolic security, however, comes at the expense of heightened glutamine metabolism to maintain glutamate availability for continuous cystine import, framing a metabolic tug-of-war.
Intriguingly, the study also discovered that perturbing cystine availability via pharmacological inhibitors or nutrient deprivation selectively sensitizes TNBC cells to glutamine deprivation. This synthetic lethal interaction reveals that disrupting this metabolic axis can critically impair cancer cell viability, suggesting a promising combinatorial therapeutic strategy. Such dual targeting could simultaneously thwart antioxidant defenses and nutrient flexibility, potentially overcoming resistance mechanisms that limit current treatments.
Further mechanistic exploration indicated that downstream of altered amino acid fluxes, key signaling pathways involved in stress response and cell fate decisions, including mTOR and integrated stress response (ISR) pathways, are modulated. These pathways coordinate metabolic adaptation, cell cycle progression, and apoptosis, amplifying the biological significance of the cystine-glutamine interplay in tumor physiology.
The potential clinical implications are profound. TNBC patients currently face limited options beyond chemotherapy. This study paves the way for designing metabolic therapies that exploit the unique amino acid dependencies of TNBC cells. For instance, inhibitors targeting system Xc⁻ or glutaminase enzymes involved in glutamine catabolism could be deployed in combination to induce metabolic collapse selectively in cancer cells while sparing normal tissues. Such precision medicine approaches have the prospect of improving patient outcomes and minimizing adverse effects.
Moreover, the metabolic vulnerabilities elucidated here may extend beyond breast cancer, given that similar dependencies on cystine and glutamine have been observed in other aggressive and treatment-resistant tumors. This universality enhances the translational potential of metabolic targeting strategies derived from these findings, possibly enabling broader applications across oncology.
The research also underscores the importance of context-dependent nutrient availability within the tumor microenvironment. Interstitial cystine concentrations vary considerably across different tissue types and pathological conditions, influencing drug efficacy and metabolic adaptation. Consequently, tailoring metabolic interventions will require integrating knowledge of tumor microenvironmental nuances alongside tumor-intrinsic metabolic traits.
In conclusion, this study represents a significant leap forward in decoding the metabolic complexity of triple-negative breast cancer. By elucidating the metabolic dialogue between exogenous cystine and glutamine dependence, it reveals weak points in the cancer’s armor ripe for therapeutic exploitation. Beyond enriching the biological understanding of tumor metabolism, the findings open promising avenues toward innovative therapies that could transform the clinical management of TNBC—a formidable adversary in the fight against breast cancer.
As cancer research continues to unravel the layers of metabolic intricacies fueling malignancy, studies like this stand at the forefront, translating molecular insights into actionable therapeutic paradigms. The prospect of harnessing metabolic dependencies to selectively eradicate resilient tumors without collateral damage heralds a new era in oncology, where precision and efficacy converge to improve lives.
Subject of Research: Metabolic interplay between exogenous cystine uptake and glutamine dependence in triple-negative breast cancer
Article Title: Metabolic interplay between exogenous cystine and glutamine dependence in triple-negative breast cancer
Article References:
Ge, Z., Wallace, M., Turner, R. et al. Metabolic interplay between exogenous cystine and glutamine dependence in triple-negative breast cancer. Cell Death Discov. 11, 430 (2025). https://doi.org/10.1038/s41420-025-02714-3
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02714-3
Tags: aggressive breast cancer subtypesamino acid metabolism in tumorscancer metabolic reprogrammingexogenous cystine uptakeglutamine dependence in cancermetabolic dependencies in TNBCmetabolic vulnerabilities in TNBCnon-essential amino acids in cancertargeted metabolic interventionstherapeutic strategies for breast cancertriple-negative breast cancertumor microenvironment challenges