A newly published study focusing on Medicare beneficiaries aged 65 and older with type 2 diabetes has identified a noteworthy association between the use of semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1 RA), and an elevated risk of nonarteritic anterior ischemic optic neuropathy (NAION). This retinal disorder, characterized by sudden vision loss resulting from impaired optic nerve head perfusion, presents a significant clinical concern especially within an aging population frequently prescribed GLP-1 RAs. The findings underscore a differential risk pattern among GLP-1 receptor agonists, with both semaglutide and liraglutide linked to higher susceptibility.
GLP-1 receptor agonists are a class of peptide-based medications widely used to manage glycemic levels in individuals with type 2 diabetes by mimicking the incretin hormone GLP-1, thereby enhancing insulin secretion and regulating blood glucose. Their cardiovascular benefits and potential weight-reduction effects have contributed to their growing use in older adults. However, the retina and optic nerve’s vascular delicacy necessitate careful pharmacovigilance as alterations in systemic hemodynamics or inflammation could predispose patients to ischemic complications.
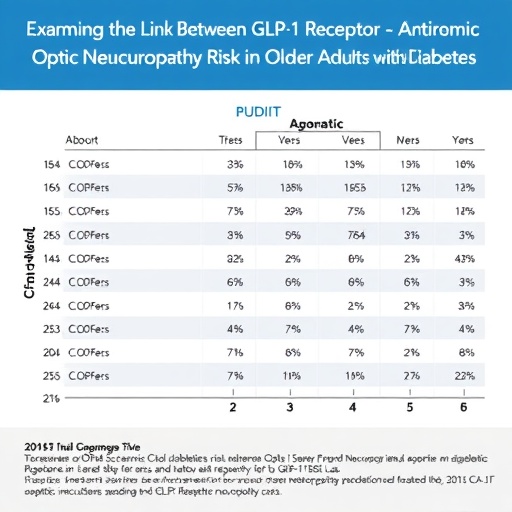
The study utilized a comprehensive Medicare database to analyze a cohort of elderly patients with type 2 diabetes, tracking the incidence of NAION among those treated with various GLP-1 RAs. By employing rigorous epidemiologic methods, the researchers adjusted for confounding factors such as age, comorbidities, baseline ophthalmologic conditions, and concurrent medication use. The statistical associations demonstrated a robust link between semaglutide exposure and increased risk of optic nerve ischemic events, with liraglutide showing a similar, albeit less pronounced, risk profile.
.adsslot_LUsgKYy0BV{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_LUsgKYy0BV{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_LUsgKYy0BV{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Nonarteritic anterior ischemic optic neuropathy results from an acute hypoperfusion event in the short posterior ciliary arteries supplying the optic nerve head, often leading to sudden monocular visual field loss. This condition is particularly prevalent in older adults with vascular risk factors, including diabetes mellitus, hypertension, and atherosclerosis. The pathophysiological mechanisms by which certain GLP-1 RAs might exacerbate ischemic vulnerability remain unclear, though hypotheses include systemic blood pressure alterations, microvascular constriction, or proinflammatory effects influenced by peptide receptor interactions.
The variation in risk observed between different GLP-1 RAs could be attributable to pharmacokinetic and pharmacodynamic differences, such as receptor affinity, half-life, and tissue distribution. Semaglutide, for example, demonstrates higher receptor binding and longer systemic exposure compared to its analogs. These factors might influence ocular microcirculation or contribute to localized ischemic insults, warranting further molecular and clinical investigation. Understanding the differential safety profiles of these agents is critical in tailoring individualized therapies for elderly diabetic patients.
This investigation also highlights the importance of close monitoring for visual symptoms in patients prescribed GLP-1 RAs, particularly semaglutide and liraglutide. Given the irreversible nature of ischemic optic neuropathy and its profound impact on quality of life, clinicians should maintain vigilance for early signs of optic nerve ischemia. Prompt recognition and possible adjustment of antidiabetic regimens may mitigate the risk of permanent visual impairment in susceptible patients.
While the study contributes valuable insights, it also leaves open questions regarding the underlying biological mechanisms, optimal screening protocols, and risk mitigation strategies for glaucoma and ischemic optic neuropathies associated with GLP-1 receptor agonists. Future research should integrate advanced imaging modalities, such as optical coherence tomography angiography (OCTA), to elucidate microvascular changes in the optic nerve head pre- and post-treatment.
Moreover, the epidemiological findings call for cross-disciplinary collaboration between endocrinologists, ophthalmologists, and neurologists to optimize the management of older adults with diabetes. Integrative approaches combining metabolic control with optic nerve health surveillance could reduce the incidence of debilitating visual outcomes attributable to ischemic neuropathies.
Clinicians should also weigh the cardiovascular and metabolic advantages of GLP-1 RAs against potential ocular risks when selecting therapeutic agents, especially in patients with preexisting optic nerve pathology or multiple vascular risk factors. The study’s insights emphasize that precision medicine must extend beyond systemic glycemic targets to encompass end-organ safety considerations, including vision.
Given the rapidly evolving pharmacotherapy landscape for diabetes, expanding post-marketing surveillance and real-world data analyses are crucial. Enhanced adverse event reporting and patient registries focusing on ocular outcomes can refine risk stratification models, guiding safer prescribing practices in aging populations vulnerable to vascular complications.
In sum, this seminal Medicare-based study reveals a significant association between semaglutide use and the risk of nonarteritic anterior ischemic optic neuropathy in patients aged 65 and older with type 2 diabetes. The findings advocate for heightened clinical awareness, individualized therapeutic decisions, and further research to unravel the complex interplay between GLP-1 receptor agonism and optic nerve vascular health.
For healthcare professionals and patients alike, these results underscore a cautious approach to incorporating newer antidiabetic agents into treatment regimens, balancing metabolic benefits with vigilant ophthalmologic monitoring to safeguard vision in the growing demographic of older adults managing type 2 diabetes.
Subject of Research: Association of GLP-1 receptor agonists, particularly semaglutide, with nonarteritic anterior ischemic optic neuropathy risk in elderly type 2 diabetes patients.
Article Title: Not specified.
News Publication Date: Not provided.
Web References: Not provided.
References: Study DOI (doi:10.1001/jamaophthalmol.2025.2299)
Image Credits: Not provided.
Keywords
Optics; Peptides; Neuropathology; Ischemia; Risk factors; Agonists; Age groups; Type 2 diabetes; Older adults; Ophthalmology; Medications; Health insurance
Tags: aging population and diabetes medicationscardiovascular benefits of GLP-1 RAsepidemiologic study of diabetes medications.GLP-1 receptor agonists and diabetesglycemic management in elderly patientsliraglutide and optic nerve healthMedicare beneficiaries and eye healthnonarteritic anterior ischemic optic neuropathy riskpharmacovigilance in diabetes treatmentretinal disorders in older adultssemaglutide and vision losssystemic hemodynamics and ischemic complications