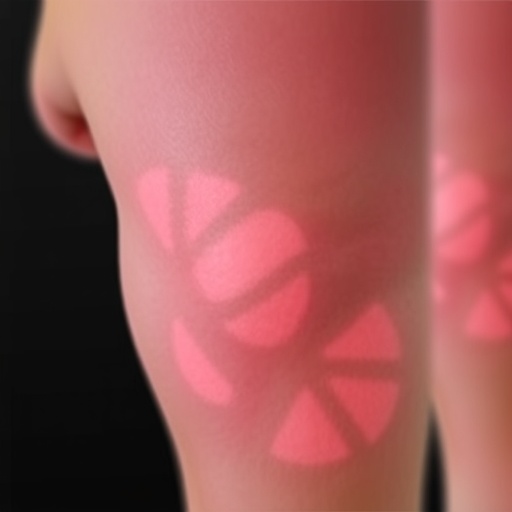
Erythromelalgia, a rare but debilitating condition marked by severe pain, redness, and heat in the extremities, has become a focal point of recent medical research. Defined by its acute episodes, which can be triggered by various factors such as heat, exertion, or even emotional stress, this disorder’s impact on daily life can be profound. A recent study published by Chen and colleagues aims to address the significant gaps in understanding the demographics and comorbidities associated with erythromelalgia, utilizing a retrospective cohort database approach.
The research presents a thorough characterization of patients suffering from this condition, revealing essential demographic trends that could inform clinical practice and future studies. It sheds light on how age, gender, and other social determinants of health interact with erythromelalgia, allowing for a more nuanced understanding of who is affected and how best to treat them. The important takeaway from the study is that erythromelalgia does not occur in isolation but frequently coexists with a range of other health issues, complicating diagnosis and treatment.
In the study, the investigators collected data from a significant sample size, ensuring that the findings would represent a meaningful cross-section of the population. The analysis identified that the majority of individuals diagnosed with erythromelalgia tend to be female, which aligns with previous findings that point to gender disparities in pain-related conditions. This might suggest underlying biological differences that warrant further investigation. Additionally, the peak age of onset appears to be during middle age, highlighting a critical window for intervention.
Co-morbid conditions were another focal point of this study, as many patients presented with overlapping health issues such as cardiovascular diseases, autoimmune disorders, and other chronic pain syndromes. The implication here is clear: erythromelalgia could be part of a larger phenotypic expression, where chronic pain is a symptom of broader systemic issues. Understanding these associations could lead to more integrated treatment approaches and better outcomes for patients.
Moreover, the researchers discussed the potential genetic and environmental factors that might predispose individuals to develop erythromelalgia. Anecdotal evidence has long suggested a familial link to the condition, but this study lays the groundwork for genetic inquiries into its pathophysiology. The role of genetics, in combination with lifestyle choices and environmental exposures, will be paramount as future research maps the etiology of erythromelalgia.
The treatments currently available are often limited and focused primarily on symptom management, leading to frustration for healthcare providers and patients alike. The study underscores the urgent need for a more comprehensive and multi-dimensional approach to managing erythromelalgia. Innovations in pain management techniques, alongside advancements in understanding the condition itself, may pave the way for more effective treatments.
One of the strengths of this study lies in its methodological rigor, utilizing a large respected database that ensures a high standard of data integrity. The retrospective design helps provide insights into the prevalence and clinical features of erythromelalgia by analyzing existing medical records. This type of research can be instrumental in identifying gaps in treatment protocols and care pathways, ultimately guiding clinicians in better managing this complex disorder.
Another essential aspect discussed in the paper is the psychological impact of erythromelalgia on patients. Persistent pain can lead to a host of mental health challenges, including depression and anxiety, creating a vicious cycle that can worsen overall health outcomes. The researchers advocate for a biopsychosocial model of care, which would integrate mental health support alongside physical health interventions, giving patients a holistic treatment framework to navigate their symptoms.
As evidenced by this exploration into erythromelalgia’s demographics and comorbidities, more visibility and resources must be dedicated to understanding and treating rare conditions. Engagement from researchers, clinicians, and patient advocates alike will be crucial in driving this agenda forward. There exists an enormous opportunity for collaboration in the scientific community to shine a light on erythromelalgia, revealing patterns that could inform broader pain management strategies applicable across various conditions.
Furthermore, the study paves the way for future research to explore specific treatment modalities that could be effective for patients with erythromelalgia. Investigating both existing therapies and novel approaches may yield new insights into how to address this challenging condition more effectively. The hope is that increased awareness and understanding will mobilize resources toward clinical trials and interventions specifically targeting erythromelalgia.
In conclusion, Chen and colleagues have provided an invaluable contribution to our understanding of erythromelalgia through their detailed investigation of the demographic and comorbid landscape of the condition. This research opens the door for further inquiry while advocating for a more nuanced approach to treatment that addresses the complexities of this often-overlooked disorder. As more attention is diverted toward rare diseases like erythromelalgia, we may begin to see a shift not only in clinical practices but in the societal perceptions surrounding chronic pain.
By disseminating these findings broadly, it fosters hope that healthcare professionals will be equipped with better tools and comprehensive strategies to manage erythromelalgia, leading to improved patient outcomes and quality of life for those affected.
Subject of Research: Erythromelalgia
Article Title: Demographics and co-morbid associations in patients with erythromelalgia: a retrospective cohort database study.
Article References:
Chen, M., Chu, D., Guo, W. et al. Demographics and co-morbid associations in patients with erythromelalgia: a retrospective cohort database study.
Arch Dermatol Res 318, 20 (2026). https://doi.org/10.1007/s00403-025-04481-8
Image Credits: AI Generated
DOI: 10.1007/s00403-025-04481-8
Keywords: Erythromelalgia, demographics, co-morbidities, chronic pain, pain management.
Tags: age and gender trends in erythromelalgiaclinical practice for erythromelalgia treatmentcomorbidities of erythromelalgiaErythromelalgia patient demographicshealth issues associated with erythromelalgiaimpact of erythromelalgia on daily liferare pain conditionsresearch on rare medical conditionsretrospective cohort studies in medicinesocial determinants of health in erythromelalgiatriggers of erythromelalgia episodesunderstanding erythromelalgia diagnosis