While it seems like restoring blood flow to an injured leg would be a good thing, it can actually cause additional damage that hinders recovery, researchers say.
While it seems like restoring blood flow to an injured leg would be a good thing, it can actually cause additional damage that hinders recovery, according to research by Drs. Babak Baban (from left), Mohamad Masoumy, and Jack Yu, all of Georgia Regents University. Photo Credit: Phil Jones, GRU Senior Photographer
Ischemia reperfusion injury affects nearly two million Americans annually with a wide variety of scenarios that temporarily impede blood flow – from traumatic limb injuries, to heart attacks, to donor organs, said Dr. Babak Baban, immunologist at the Medical College of Georgia and College of Dental Medicine at Georgia Regents University.
Restoring blood flow actually heightens inflammation and cell death rather than recovery for many of these patients.
“Think about trying to hold onto a nuclear power plant after you unplug the electricity and cannot pump water to cool it down,” said Dr. Jack Yu, Chief of MCG’s Section of Plastic and Reconstructive Surgery. “All kinds of bad things start happening.”
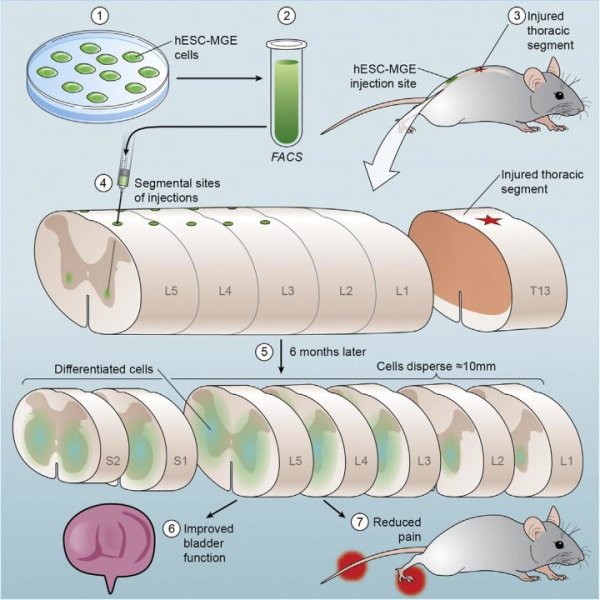
Baban and Yu are collaborators on a study published in the journal PLOS ONE that shows one way stem cell therapy appears to intervene is with the help of an enzyme also used by a fetus to escape rejection by the mother’s immune system.
Earlier studies indicate stem cells may improve recovery both by enabling new blood vessel growth and by turning down the now-severe inflammation, Baban said. The new study shows that indoleomine 2,3 dioxygenase, or IDO, widely known to dampen the immune response and create tolerance, plays an important role in regulating inflammation in that scenario. Stems cells and numerous other cell types are known to express IDO.
In fact, IDO boosted stem cell efficacy by about a third in their studies in animal models comparing the therapy in normal mice versus mice missing IDO. The researchers documented decreased expression of inflammatory markers, swelling and cell death, which correlate with a shorter, improved recovery.
That could be just what the doctor ordered for these patients, said Baban, the study’s corresponding author. “We don’t want to turn off the immune system, we want to turn it back to normal,” he said.
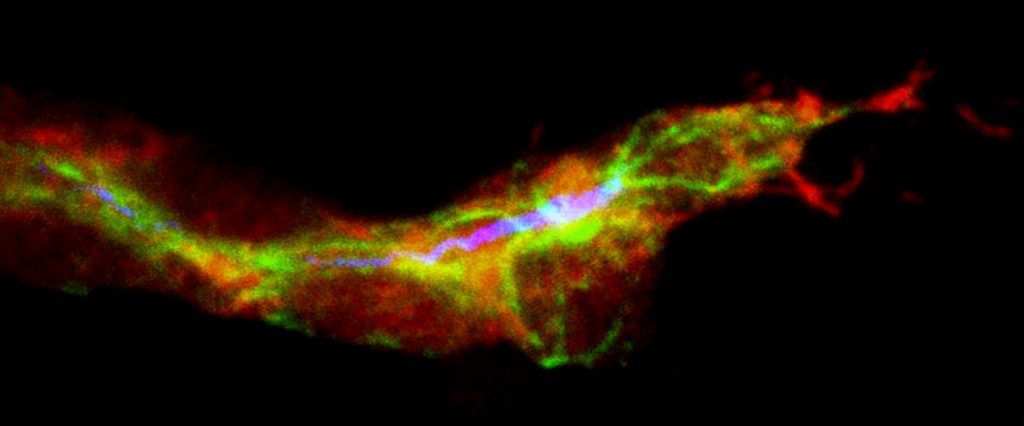
Problems start with even a short period of inadequate blood and nutrients resulting in the rapid accumulation of destructive acidic metabolites, free radicals, and damage to cell structures, Yu said. Cell power plants, called mitochondria, which should be producing the energy source ATP, are among the early casualties, quickly becoming fat, leaky, and dysfunctional.
“The mitochondria are sick; they are very, very sick,” Yu said. When blood flow is restored, it can put huge additional stress on sick powerhouses.
“They start to leak things that should not be outside the mitochondria,” he said. Without adequate energy and with leaky powerhouses, cells quickly succumb. Inflammation, which is part of the normal healing process, escalates to help clean up the mess, but instead further exacerbates the problem.
While their findings were in limb injuries, the researchers say they should translate to the myriad of scenarios resulting in reperfusion injury. In fact, in just a short two hours in the operating room, Yu has seen free flaps, where tissue is moved from one area of the body to another to cover a burn or rebuild a breast, start dying from ischemia reperfusion injury.
“It cuts across many, many individual disease conditions,” Yu said. Transplant centers already are experimenting with pulsing donor organs to avoid reperfusion trauma.
Next steps include seeing if more is better, by giving more stem cells – the researchers only gave one dose in the studies – as well as IDO-enhancing drugs, Baban said. This will include incubating stem cells with IDO, Baban said.
The researchers note that stem cell therapy isn’t yet used to help patients’ injured limbs recover, but is being studied clinically to aid stroke and heart attack recovery at MCG and other centers. Right now, the most physicians can do is restore blood flow and give broad-spectrum antibiotics.
“Sometimes it works, sometimes it doesn’t,” Yu said. “That is why this kind of pharmacologic intervention could be very, very important.
Endogenous stems cells enable the body to replace cells that are lost to wear and tear and aging. IDO is one of numerous immune modulators in the body. It remains unclear whether some individuals have higher IDO levels.
Story Source:
The above story is based on materials provided by Medical College of Georgia at Georgia Regents University, Toni Baker.