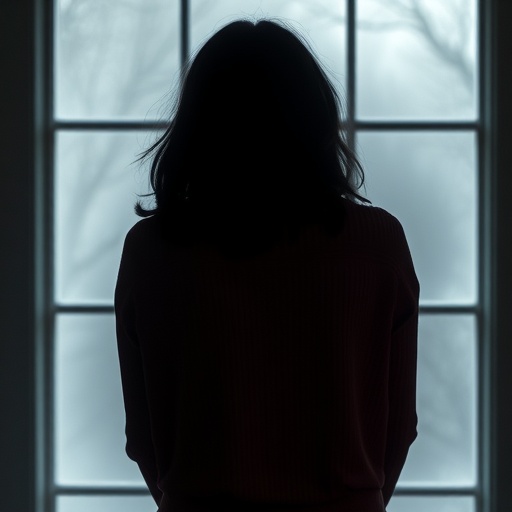
A groundbreaking new study from Karolinska Institutet sheds light on a profoundly concerning issue within psychiatric care: individuals subjected to involuntary hospitalization face a markedly elevated risk of suicide after discharge. Published recently in The Lancet Regional Health – Europe, this extensive research underscores the critical necessity for enhanced post-discharge support and vigilance within mental health services. By meticulously analyzing nationwide data, the study offers a compelling quantitative foundation emphasizing that the period following compulsory psychiatric treatment is a pivotal vulnerability window for suicide risk.
Each year, over 10,000 individuals in Sweden undergo involuntary psychiatric hospitalization—a severe intervention reserved for those with acute mental disorders who refuse treatment despite the urgent need for care. This study specifically targeted this population, tracing their outcomes over an average span exceeding four years. Strikingly, among the 72,000+ patients followed, more than two thousand died by suicide, making the mortality rate in this group alarmingly high and demanding immediate attention from public health frameworks and psychiatric protocols.
One of the most alarming revelations is the temporal pattern of suicide risk post-discharge. Researchers identified that suicide risk is at its zenith during the first month following release from involuntary care, a critical timeframe that demands intensified clinical and social intervention. Importantly, while this heightened risk tapers somewhat, it remains substantially elevated for several subsequent years, signifying the enduring impact of severe psychiatric episodes and the insufficiency of current aftercare models.
When compared to patients who underwent voluntary psychiatric hospitalization, the data illustrates a 1.6-fold increase in suicide risk among those treated involuntarily. More starkly, when juxtaposed against psychiatric outpatients and the general population, these figures escalate to nearly four times and fifty-six times higher, respectively. These comparisons underscore the profound severity and chronicity of conditions afflicting this group, highlighting that involuntary hospitalization is more than just a marker of immediate crisis; it is indicative of long-term vulnerability.
Demographic and clinical factors further modulate this risk landscape. The study pinpointed subgroups with disproportionately increased suicide risk, notably young men and individuals without partners, underscoring the complex interplay between social isolation and mental health crises. Additionally, diagnoses such as personality disorders and substance use disorders emerged as significant predictors of elevated suicide risk, compounding the challenges of managing these conditions in post-discharge settings.
Moreover, previous interactions with involuntary treatment protocols and documented histories of self-harm were found to exacerbate this risk, suggesting that repetitive cycles of acute psychiatric episodes and institutionalization might contribute to an entrenched risk trajectory. Such insights advocate for a more nuanced understanding of patient histories and tailored interventions targeting known risk factors within psychiatric populations.
The study’s authors caution, however, that despite the clear association between involuntary treatment and increased suicide risk, causality cannot be definitively established due to the observational nature of the research. Involuntary hospitalization itself is unlikely to be a direct cause of suicide; rather, it serves as an important risk marker, reflecting the profound severity and complexity of underlying psychiatric illnesses and social circumstances.
These findings bear critical implications for psychiatric practice and health policy. Effective post-discharge strategies, encompassing comprehensive risk assessment, structured follow-up, psychosocial support, and crisis intervention services, are imperative to mitigate suicide risk. The research team is actively pursuing further investigation into whether risk stratification models based on these findings can inform clinical decision-making around discharge timing and personalized aftercare plans.
Collaborative efforts enhancing the continuity of care between inpatient services and community-based mental health providers represent a key therapeutic frontier. Integration of evidence-based suicide prevention frameworks within routine psychiatric practice will be vital to addressing this urgent public health challenge and reducing preventable mortality among this vulnerable group.
The data utilization pipeline for this study was extensive, drawing on numerous national registries and enriched by international collaborations with academic institutions such as the University of Oxford and Indiana University. These partnerships facilitated robust data validation and broadened the generalizability of findings, ensuring the study’s relevance extends beyond Sweden’s borders.
Funding was provided by authoritative bodies, including the Swedish Research Council and the Söderström-Königska Foundation, emphasizing the strategic prioritization of mental health research within global scientific and health communities. The authors are transparent regarding potential conflicts of interest, maintaining rigorous ethical standards customary for high-impact scientific publications.
Ultimately, this landmark study articulates a compelling call to action for healthcare professionals, policymakers, and society at large. The intersection of involuntary psychiatric care and suicide risk is complex, multifaceted, and deeply consequential. Addressing these vulnerabilities necessitates a systemic shift toward more compassionate, coordinated, and continuous mental healthcare models that can effectively safeguard those most at risk during one of the most precarious phases of their recovery journey.
Subject of Research: People
Article Title: Suicide after involuntary psychiatric care: a nationwide cohort study in Sweden
News Publication Date: 4-Nov-2025
Web References: http://dx.doi.org/10.1016/j.lanepe.2025.101504
References: Grossmann L, Johansson F, Fazel S, Kuja-Halkola R, Bråstad B, Mataix-Cols D, Fernández de la Cruz L, Runeson B, Lichtenstein P, Chang Z, Larsson H, Brikell I, D’Onofrio B, Pingel R, Rück C, Wallert J. Suicide after involuntary psychiatric care: a nationwide cohort study in Sweden. The Lancet Regional Health – Europe. 2025 Nov 4; DOI:10.1016/j.lanepe.2025.101504
Keywords: Suicide, Mental health facilities, Mental health, Psychiatric disorders, Psychiatry
Tags: acute mental disorderscritical care transition in psychiatryelevated suicide riskinvoluntary psychiatric treatmentlongitudinal study on suicidemental health intervention outcomesmental health servicespost-discharge supportpsychiatric hospitalization statisticspublic health implicationssuicide prevention strategiesvulnerable populations in mental health