Credit: CHEST
Glenview, IL, May 24, 2018 – The rising incidence of sepsis, a leading cause of in-hospital death, has prompted the Centers for Medicare and Medicaid Services (CMS) to issue protocols known as care bundles to standardize and improve sepsis care. Because of a known association between elevated lactate levels and increased mortality, the guidelines mandate that lactate levels should be tested soon after the onset of sepsis. A new study in the journal CHEST® found that a significant proportion of patients with suspected sepsis do not have their lactates measured within the recommended timeframe. These patients experienced delayed antibiotic therapy and IV fluid administration, as well as increased risk of in-hospital death.
According to first author Xuan (Susan) Han, MD, Department of Medicine, University of Chicago, Chicago, IL, USA, "Sepsis continues to be a major public health problem in the US, one with persistently high mortality despite continued efforts to improve care. Our goal with this study was to better understand, on a more granular level, how sepsis bundles affect the patients we apply them to."
The guidelines, issued in 2015 by the CMS, are SEP-1 (Severe Sepsis and Septic Shock Early Management Bundle). One of the recommendations is the measurement of serum lactate between six hours before and three hours after severe sepsis presentation, followed by a repeat within six hours of presentation if the initial lactate is elevated.
"Systematic early lactate measurements in patients presenting with sepsis would result in a significant increase in the number of lactates measured on patients but may be of benefit in identifying patients with elevated initial lactates who are at risk for poorer outcomes. Patients with early lactate measurements received earlier interventions such as antibiotic administration, which is known to improve mortality in sepsis," explained Matthew M. Churpek, MD, MPH, PhD, of the Department of Medicine and Center for Healthcare Delivery, Science and Innovation at the University of Chicago, Chicago, IL, USA.
To see what was being done in actual clinical practice, researchers at the University of Chicago reviewed the records of close to 150,000 patients admitted to a single tertiary care academic hospital from November 2008 to January 2016. Information regarding each patient's characteristics, vital signs, laboratory measurements, and medical therapy was analyzed. There was a particular focus on lactate measurements and levels.
They identified 5,762 admissions that met the three SEP-1 criteria for severe sepsis within a six-hour period. Of these, only 60 percent had an initial lactate drawn within the SEP-1 specified timeframe. Fourteen percent had their levels measured between three and 24 hours after the time of first suspicion of sepsis ("delayed lactates"), and more than one quarter had no lactate measurements at all.
Whether lactates were measured promptly varied with where the patient was being treated. Seventy-nine percent of patients treated in the emergency department had levels measured within the specified time period compared with 55 percent in the intensive care unit (ICU) but only 32 percent in hospital wards. "Our study demonstrates that a large number of patients become newly septic on the wards. This is an important population of patients in which to effectively and quickly identify and treat sepsis," commented Dr. Churpek.
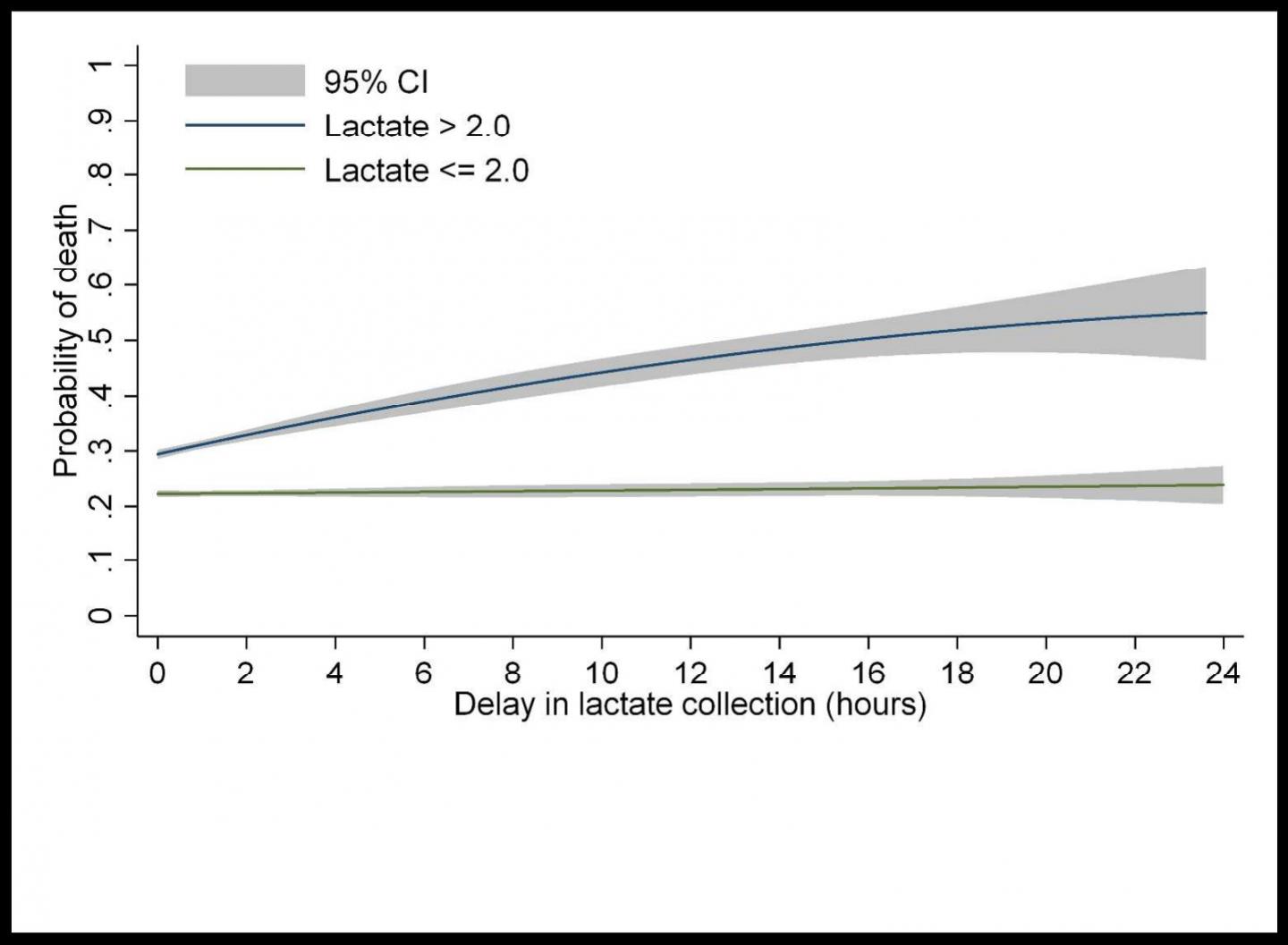
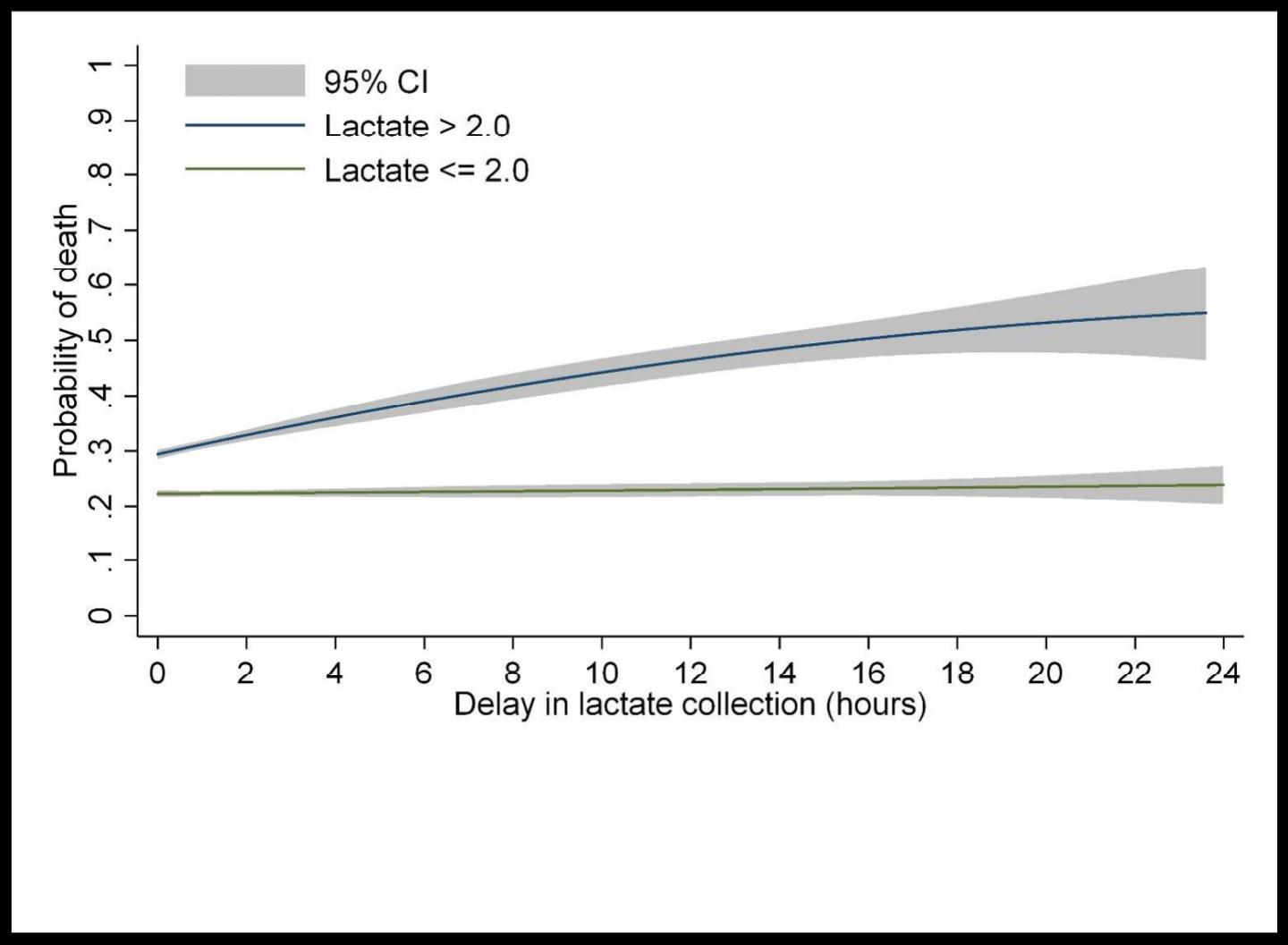
Mortality increased with higher initial lactate levels. For example, in the ICU, the mortality rate was 35 percent for patients with a normal initial lactate level compared with 62 percent for those with elevated lactate levels. Most troubling, in patients with elevated lactate levels at the first draw, each hour of delay was associated with a 2 percent increase in the odds of in-hospital death. Importantly, it took approximately twice as long for patients with delayed lactate measurements to receive antibiotics and more than three times as long for them to receive fluids when compared with patients who had lactates drawn within the SEP-1 window.
"The SEP-1 bundle is the most recent national effort at standardizing and improving sepsis care, but the evidence supporting its various measures is mixed or lacking. In addition, SEP-1 has been highly controversial. This study better characterized the patients affected by SEP-1, as well as the impact of one component of SEP-1, lactate measurement, on hospitalized patients. Systematic early lactate measurements when a patient presents with sepsis may thus be useful in prompting earlier, potentially life-saving interventions," added Dr. Churpek.
###
Media Contact
Andrea Camino
[email protected]
224-521-9513
@elseviernews
http://www.elsevier.com
Related Journal Article
http://dx.doi.org/10.1016/j.chest.2018.03.025