In a groundbreaking study set to redefine therapeutic strategies in oncology, researchers have unveiled a potent combination therapy targeting p53-mutant diffuse large B-cell lymphoma (DLBCL), one of the most aggressive forms of non-Hodgkin lymphoma. This malignancy, notorious for its resistance to conventional treatments, presents a daunting challenge due to the frequent mutation of the tumor suppressor gene p53. The novel approach involves the synergistic use of histone deacetylase (HDAC) inhibitors and phosphoinositide 3-kinase (PI3K) inhibitors, which together orchestrate a suppression of autophagy and trigger apoptosis through the stabilization of cytoplasmic IκBα. This mechanism uncovers a new axis of vulnerability in cancer cells harboring p53 mutations, providing a promising avenue for clinical translation.
Diffuse large B-cell lymphoma represents a complex pathophysiological entity characterized by a diverse molecular landscape and varying responses to treatment. The mutant forms of p53 found in these tumors typically confer aggressive growth and resistance to apoptosis, thereby undermining the efficacy of chemotherapy and radiation. In this study, the interplay between epigenetic modulators and key signaling pathways was explored to dismantle the survival mechanisms of these malignant cells. HDAC inhibitors, known to alter chromatin structure and gene expression, were combined with PI3K inhibitors, which block a crucial intracellular signaling cascade involved in cell proliferation and survival.
What distinguishes this research is the identification of cytoplasmic IκBα stabilization as the lynchpin for the combined treatment’s pro-apoptotic effect. IκBα, an inhibitor of the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, plays a critical role in regulating inflammation, immunity, and cell survival. Typically, NF-κB activity is heightened in cancer, promoting tumor growth and resistance to cell death. The dual inhibition leads to accumulation of IκBα in the cytoplasm, effectively blocking NF-κB signaling and tipping the balance toward apoptosis. This strategic blockage interrupts the tumor cells’ ability to evade programmed cell death, a hallmark of cancer progression.
Autophagy, a cellular recycling process that tumors exploit for survival under metabolic stress, is also substantially impacted by this therapeutic combination. While autophagy can be a double-edged sword in cancer, its suppression in p53-mutant DLBCL emerged as a critical factor in enhancing cell death. By inhibiting both HDAC and PI3K, researchers demonstrated a substantial reduction in autophagic flux, depriving the malignant cells of a vital survival mechanism. This dual blockade not only sensitizes the cells to apoptosis but also prevents the usual compensatory survival pathways from taking over.
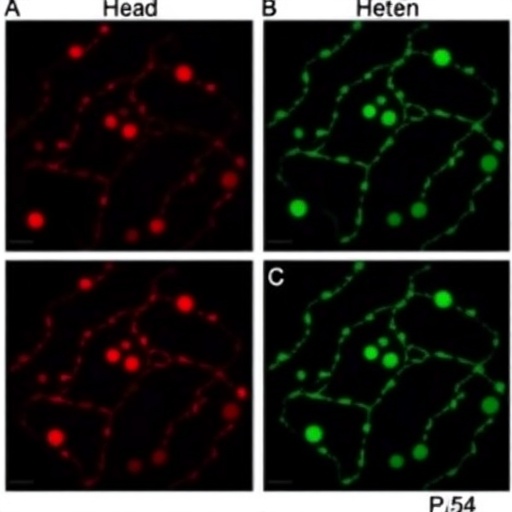
The intricate crosstalk between epigenetic modulation and intracellular signaling cascades revealed in this study points to a sophisticated mechanism by which malignant cells can be hijacked. Methodologically, the researchers employed a comprehensive array of molecular biology techniques, including Western blotting, immunofluorescence, flow cytometry, and autophagy flux assays, to dissect the effects of the inhibitors alone and in combination. These robust approaches substantiated the hypothesis that the combined regimen elevates cytoplasmic IκBα, suppresses autophagy, and triggers apoptotic pathways more effectively than either drug alone.
Importantly, the therapeutic combination demonstrated specificity toward p53-mutant DLBCL cells, sparing non-malignant cells, which underscores the potential for reduced systemic toxicity in clinical applications. This specificity is critical in oncology to maximize efficacy while minimizing collateral damage to healthy tissues. Future clinical trials will be pivotal in assessing the translational capacity of this treatment, particularly in patient cohorts characterized by poor prognosis due to p53 mutations.
The PI3K pathway, a central player in cell growth and metabolism, has long been targeted in cancer therapy, but its clinical success has been hampered by resistance and side effects. Similarly, HDAC inhibitors have shown efficacy but often produce transient responses when used as monotherapies. This research elegantly demonstrates that their combination exploits complementary mechanisms—epigenetic reprogramming and signal transduction inhibition—to deliver a potent blow to tumor cell viability.
One of the most compelling aspects of this study is its elucidation of the mechanistic underpinnings governing the treatment response. Cytoplasmic IκBα stabilization emerges not merely as a byproduct of drug action but as a pivotal mediator that bridges epigenetic regulation and survival signaling. By preventing the degradation of IκBα, the therapy maintains the inhibitor in the cytoplasm, preventing NF-κB translocation to the nucleus and subsequent transcription of survival genes.
Beyond the molecular intricacies, this discovery has significant implications for the wider oncology community. It challenges the existing paradigms that prioritize targeting nuclear pathways and emphasizes the cytoplasmic sequestration mechanisms as viable intervention points. It also revitalizes the search for combinational treatments that can overcome the adaptive resistance seen in refractory cancers.
The suppression of autophagy not only enhances apoptosis but also sensitizes tumor cells to existing therapies, suggesting that this combined regimen could be integrated with standard chemotherapeutic agents to improve outcomes further. The rationale is supported by evidence indicating that autophagy inhibition may prevent tumor cells from entering dormancy or evading drug-induced stress.
While this study concentrates on p53-mutant diffuse large B-cell lymphoma, the principles uncovered may be extrapolated to other malignancies characterized by similar molecular aberrations. Given that p53 mutations are prevalent across numerous cancer types, the strategy of dual HDAC and PI3K inhibition alongside modulating IκBα offers a versatile template for future drug development.
Clinical translation will necessitate addressing challenges such as drug dosing, scheduling, and managing potential toxicities arising from combined inhibition. However, the specificity for p53-mutant cells bodes well for an acceptable therapeutic window. Additionally, the molecular signatures identified in this study could serve as biomarkers to stratify patients who would benefit most from such an approach.
The work spearheaded by Yao, Li, Jiang, and colleagues represents a significant leap toward precision medicine in oncology, harnessing the convergence of epigenetic and signaling pathway modulation to overcome therapy resistance. Their findings offer new hope for patients afflicted with aggressive lymphoma subtypes that currently have limited treatment options, indicating that the future of cancer therapy lies in intricate, multi-targeted regimens.
As the field moves forward, incorporating such combinational strategies into clinical trial designs will be crucial to validate efficacy and safety in diverse patient populations. The potential to transform lethal cancers into manageable or even curable diseases hinges on our understanding of and ability to manipulate these complex molecular networks.
In conclusion, this pioneering study elucidates a novel and effective therapeutic avenue for p53-mutant diffuse large B-cell lymphoma. By co-targeting HDAC and PI3K and leveraging cytoplasmic IκBα stabilization to disrupt autophagy and promote apoptosis, the researchers have opened a new frontier in cancer treatment. This dual inhibition strategy exemplifies the power of molecular synergy in disabling cancer’s defense mechanisms and sets the stage for innovative clinical interventions that could dramatically improve patient survival and quality of life.
Subject of Research: Combination therapy using HDAC inhibitor and PI3K inhibitor to induce apoptosis and suppress autophagy in p53-mutant diffuse large B-cell lymphoma
Article Title: Combination of HDAC inhibitor and PI3K inhibitor suppresses autophagy and induces apoptosis via cytoplasmic IκBα stabilization in p53-mutant diffuse large B-cell lymphoma
Article References:
Yao, J., Li, M., Jiang, Y. et al. Combination of HDAC inhibitor and PI3K inhibitor suppresses autophagy and induces apoptosis via cytoplasmic IκBα stabilization in p53-mutant diffuse large B-cell lymphoma. Cell Death Discov. 11, 445 (2025). https://doi.org/10.1038/s41420-025-02756-7
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02756-7
Tags: aggressive non-Hodgkin lymphoma treatmentapoptosis induction in lymphomaautophagy suppression in cancer cellsclinical translation of cancer therapiescytoplasmic IκBα stabilizationdual HDAC and PI3K inhibitorsepigenetic modulation in cancernovel cancer combination therapyp53-mutant diffuse large B-cell lymphomaresistance to chemotherapy in DLBCLsignaling pathways in lymphoma treatmenttherapeutic strategies in oncology