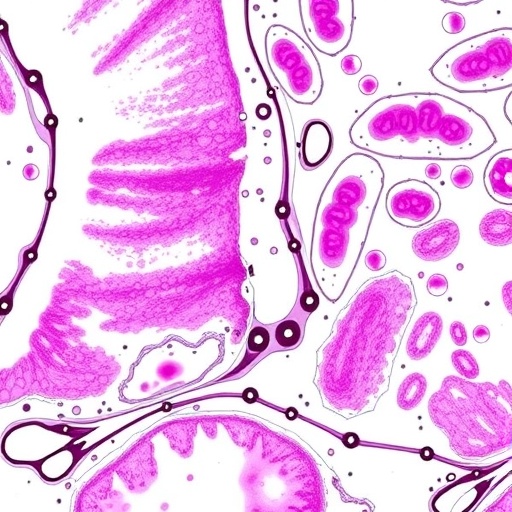
A groundbreaking multicenter study has unveiled a novel approach employing deep learning to decode complex genetic alterations within colorectal cancer, marking a significant advancement in precision oncology. Researchers analyzed nearly 2,000 digitized tissue slides from colon cancer patients across seven independent cohorts in Europe and the United States, integrating whole-slide histological images with detailed clinical, demographic, and lifestyle datasets. This extensive dataset enabled the development of a sophisticated “multi-target transformer model” capable of simultaneously predicting a broad spectrum of genetic mutations directly from standard stained tissue sections — a feat that outperforms previous models traditionally limited to single-target mutation prediction.
The innovative model represents a leap forward from prior deep learning frameworks by addressing the co-occurrence of genetic mutations and shared morphological features within tumors. Earlier AI systems largely focused on identifying one mutation at a time, missing the intricate interplay and combined phenotypic manifestations that multiple concurrent genetic aberrations produce. By capturing shared visual patterns that correlate with multiple genetic markers, the model lays the groundwork for more holistic and nuanced interpretations of tumor biology right from histopathological images, offering insights previously accessible primarily through expensive and time-intensive molecular testing.
Marco Gustav, M.Sc., the study’s lead author and a research associate at the Else Kröner Fresenius Center for Digital Health (EKFZ) at TU Dresden, explains, “Our transformer model detects numerous biomarkers concurrently, including mutations that have not yet attained clinical relevance. This comprehensive identification is made feasible by recognizing shared tissue morphology changes, particularly prevalent in microsatellite instability (MSI)-high tumors—a critical subtype of colorectal cancer.” MSI describes a molecular condition resulting from defective DNA repair systems, leading to unstable repetitive DNA sequences, a hallmark linked with distinct therapeutic responses, especially to immunotherapy.
.adsslot_Ke4qRcokDO{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_Ke4qRcokDO{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_Ke4qRcokDO{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Microsatellite instability (MSI) is a pivotal factor in colorectal cancer diagnostics and treatment stratification, given its association with better responses to immune checkpoint inhibitors. Detecting MSI status directly from pathology slides using AI could revolutionize clinical workflows, providing rapid, cost-effective preliminaries without waiting for molecular assays. The ML model’s capability extends beyond just MSI detection to encompass key driver mutations, such as those in the BRAF and RNF43 genes, which are essential for prognostication and targeted treatment decisions. The model’s performance matches or even surpasses traditional single-target predictive frameworks, underscoring the power of embracing multi-target learning strategies.
An integral aspect of the study was its collaborative nature, integrating pathology expertise to ensure rigorous assessment of tissue morphology and validate AI outputs. Dr. Nic G. Reitsam, a pathologist affiliated with the Medical Faculty at the University of Augsburg, contributed critical domain knowledge that anchored the model’s development in practical and clinically relevant contexts. This interplay between computational scientists and experienced medical specialists exemplifies a growing trend where digital pathology and machine learning converge to redefine diagnostic paradigms.
Jakob N. Kather, Professor of Clinical Artificial Intelligence at EKFZ and senior oncologist at the National Center for Tumor Diseases and University Hospital Carl Gustav Carus Dresden, highlights the transformative potential: “By accelerating diagnostic routines and unveiling intricate genotype-phenotype relationships, AI-driven methodologies can refine patient selection methods for molecular testing and tailor personalized therapeutic approaches. Our work points to a future where integrated digital tools form a cornerstone of oncology practice.” This vision embodies precision medicine, where treatments and prognoses are finely tuned to a tumor’s unique molecular and phenotypic landscape.
The methodological core—the multi-target transformer architecture—derives from recent advances in natural language processing adapted for medical image analysis. This architecture attentively processes entire histology slides, recognizing contextual morphological cues linked to various mutations without requiring prior knowledge of each mutation’s individual effects. Such holistic image interpretation contrasts starkly with older machine learning methods that isolated features or required manual region-of-interest selection, limiting comprehensiveness and robustness.
Testing the model across multiple independent cohorts in geographically and demographically diverse populations further solidified its generalizability and clinical relevance. The inclusion of centers from the Medical University of Vienna, Fred Hutchinson Cancer Center, Mayo Clinic, University of Augsburg, and NCT Heidelberg ensured that findings are broadly applicable and not confined to a single institutional setting. This wide collaboration also facilitated access to rich datasets harmonizing histopathology and clinical metadata, a prerequisite for reliable deep learning analyses in oncology.
The study’s implications extend beyond colorectal cancer. By successfully decoding complex genotype-phenotype correlations in this common cancer type, the research paves the way for applying similar deep learning models to other malignancies where genetic heterogeneity and histological variability complicate diagnosis and treatment. Future iterations of the model could incorporate a broader array of biomarkers and integrate multi-modal data such as radiological images, further enriching predictive accuracy.
Clinical integration of these AI tools promises to trim turnaround times for pathology reports, reduce costs associated with comprehensive molecular profiling, and potentially improve patient outcomes through earlier and more tailored interventions. However, prospective clinical trials remain vital to establishing standardized protocols and regulatory approvals for routine practice. Ethical considerations, including data privacy, algorithm transparency, and equitable access, also warrant concerted attention as AI technologies become embedded in healthcare.
Furthermore, the EKFZ for Digital Health itself represents an innovative institutional model, funded generously by the Else Kröner Fresenius Foundation to foster cross-disciplinary digital health research. Since its establishment in 2019 at TU Dresden and the University Hospital Carl Gustav Carus Dresden, EKFZ has cultivated an environment where computational innovation and clinical expertise synergize to address pressing medical challenges, as exemplified by this landmark colorectal cancer study.
Altogether, this study exemplifies how cutting-edge artificial intelligence can decode the complex molecular tapestry of cancer from routine clinical materials, shifting diagnostic paradigms and opening avenues for personalized medicine. As researchers build upon this foundation, deep learning’s role in oncology is poised to grow, yielding profound impacts on patient care and outcomes.
Subject of Research: Deep learning-based prediction of genotype–phenotype correlations in colorectal cancer using histopathological images
Article Title: Assessing genotype−phenotype correlations in colorectal cancer with deep learning: a multicentre cohort study
News Publication Date: 18-Aug-2025
Image Credits: Anja Stübner / EKFZ
Keywords: Cancer, Colorectal cancer, Diseases and disorders, Computer science, Artificial intelligence
Tags: advanced AI frameworks for tumor biologyAI in colorectal cancer researchco-occurrence of genetic mutations in cancerdeep learning in precision oncologydigitized tissue slides for cancer diagnosishistological analysis of tissue samplesinnovations in molecular testing for cancer detectionintegrating clinical datasets with histopathologymulti-target transformer model for genetic mutationsnovel approaches in cancer mutation predictionpersonalized medicine and cancer treatmentsimultaneous detection of cancer markers