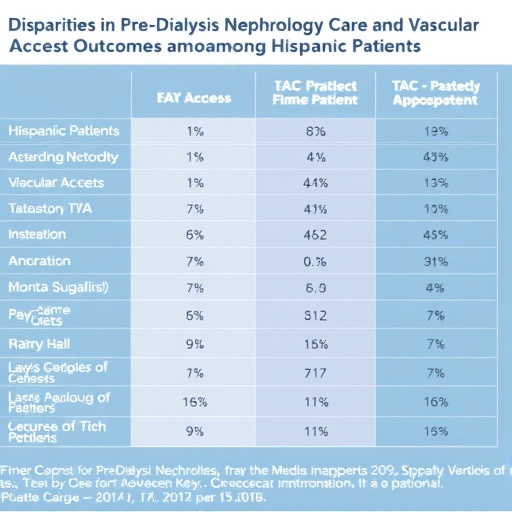
A recent retrospective cohort study has shed new light on the persistent disparities faced by Hispanic patients initiating hemodialysis, revealing that systemic barriers in pre-dialysis nephrology care play a pivotal role in these inequities. The research, published in the esteemed journal JAMA Network Open, meticulously analyzed patient data to uncover how differences in early access to specialist care directly contribute to approximately one-third of the vascular access disparities experienced by Hispanic individuals at the onset of dialysis treatment.
The management of vascular access is a critical determinant of outcomes for patients with end-stage kidney disease (ESKD) undergoing hemodialysis. Optimal vascular access, such as arteriovenous fistulas or grafts, is associated with better clinical outcomes, reduced infection rates, and improved long-term survival. However, disparities in the timely placement and use of these access types have long been documented, particularly within minority populations, leading to worse prognoses and an increased reliance on central venous catheters, which carry significant risk.
Central to the study’s findings is the revelation that systemic factors within healthcare delivery infrastructures disproportionately hinder early nephrology referral and assessment among Hispanic patients. Early nephrology care is critical for preparing patients for dialysis, enabling timely vascular access planning and improving treatment trajectories. Delays often result in emergency dialysis initiations, which exacerbate vascular access complications and clinical morbidity.
This investigation employed robust statistical methodologies on a large cohort of newly diagnosed hemodialysis patients, stratifying the data by ethnicity and adjusting for relevant confounders including socioeconomic status, comorbid conditions, and healthcare utilization patterns. The researchers were able to isolate the extent to which healthcare system deficiencies, rather than patient-level factors alone, accounted for disparities in vascular access type at dialysis initiation.
Importantly, the study emphasizes the impact of healthcare policy and system design on equitable outcomes. It suggests that addressing these systemic barriers is not solely a matter of patient education or individual compliance but requires transformative policy interventions that improve timely nephrology referrals and access to specialty care among Hispanic populations. Such strategies could encompass enhanced care coordination, culturally tailored outreach programs, and systemic accountability measures.
Beyond highlighting disparities, the research offers a blueprint for targeted remedies. By quantifying the proportion of access inequity attributable to system-based delays, it calls for deployment of evidence-driven policy initiatives that prioritize early kidney disease detection and care navigation in vulnerable communities. The authors stress that these interventions could substantially reduce preventable complications associated with suboptimal vascular access.
From a physiological standpoint, the study situates vascular access as the nexus of clinical functionality and patient safety in hemodialysis. The complexities of creating and maintaining reliable access are well-documented, involving vascular biology, surgical technique, and patient-specific factors. However, systemic lapses in nephrology service access undermine these clinical efforts, compounding biological and social determinants of health to amplify disparities.
The broader implications of these findings resonate deeply within nephrology and health equity domains. Kidney failure incidence is disproportionately high among Hispanic populations, a trend exacerbated by socioeconomic inequities and social determinants of health. Addressing pre-dialysis healthcare access gaps is thus a critical axis for reducing morbidity and mortality in this group, while aligning with national objectives of equitable healthcare delivery.
This study’s innovative focus on system-level contributors complements prior research that has largely concentrated on patient-level or biological explanations for disparities in kidney disease outcomes. By illuminating structural barriers within healthcare delivery, it invites a paradigm shift toward systemic reform and collaborative policy-making among healthcare providers, insurers, and public health entities.
Practically, the advancement of nephrology referral protocols and the integration of multidisciplinary care models could serve as effective modalities to bridge these access gaps. Proactive screening initiatives, enhanced electronic health record prompts, and community-based interventions tailored to Hispanic populations could collectively improve early nephrology engagement, thereby optimizing vascular access planning.
The study also underscores the critical necessity for culturally competent care frameworks that recognize and address linguistic, cultural, and socioeconomic hurdles impeding timely nephrology access. Employing community health workers and patient navigators skilled in culturally specific communication could mitigate these barriers and foster trust in healthcare systems.
Furthermore, the research findings lay the groundwork for future investigations to probe the complex interactions between healthcare systems, social determinants, and patient outcomes in chronic kidney disease management. Longitudinal studies and interventional trials are needed to validate and extend these insights, ultimately informing scalable strategies for health equity in nephrology care.
In conclusion, this retrospective cohort study offers compelling evidence that pre-dialysis nephrology care disparities substantially contribute to vascular access inequities among Hispanic individuals initiating hemodialysis. The findings call for systemic, policy-driven remedies focused on early identification and timely referral to nephrology services. In doing so, the research delineates a clear path toward reducing disparities, improving clinical outcomes, and advancing health equity in kidney failure care.
Subject of Research: Healthcare system disparities in pre-dialysis nephrology access and their impact on vascular access outcomes among Hispanic hemodialysis patients.
Article Title: Not specified.
News Publication Date: Not specified.
Web References: Not available.
References: DOI 10.1001/jamanetworkopen.2025.30972
Image Credits: Not provided.
Keywords: Nephrology, Vascular biology, Health care, Ethnicity, Health care policy, Kidney, Hemodialysis
Tags: arteriovenous fistulas and graftscentral venous catheters riskschronic kidney disease managementdisparities in nephrology careearly nephrology referralend-stage kidney diseaseHispanic patients in hemodialysisJAMA Network Open studyminority health disparitiessystemic barriers in healthcaretimely placement of vascular accessvascular access outcomes