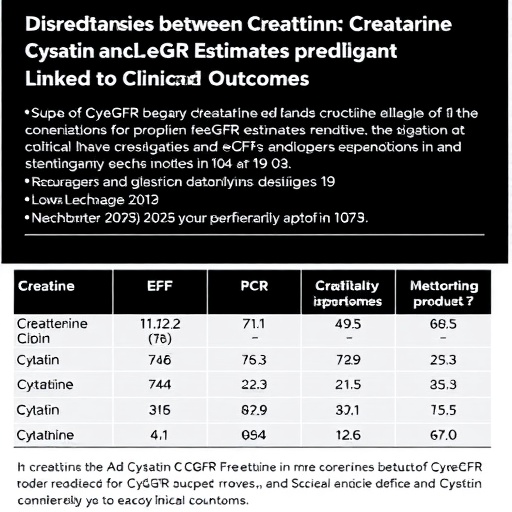
In a groundbreaking revelation from the Chronic Kidney Disease Prognosis Consortium, recent analyses indicate a striking discrepancy between two commonly used measures of kidney function—the cystatin C–based estimated glomerular filtration rate (eGFRcys) and the creatinine-based estimated glomerular filtration rate (eGFRcr). The study highlights that approximately 11% of outpatients and 35% of hospitalized individuals exhibit eGFRcys values that are at least 30% lower than their corresponding eGFRcr measurements. This divergence, far from being a mere biochemical anomaly, correlates strongly with adverse clinical outcomes, including elevated risks of all-cause mortality, cardiovascular events, and progression to kidney failure.
The glomerular filtration rate (GFR) serves as the paramount indicator of renal function, traditionally estimated through serum creatinine levels due to its widespread availability and cost-effectiveness. However, creatinine concentration is influenced by variables such as muscle mass, diet, and medications, sometimes confounding its accuracy. Cystatin C, a low molecular weight protein produced at a constant rate by all nucleated cells, offers an alternative biomarker less affected by non-renal factors. This study capitalizes on the contrast between these two biomarkers to uncover hidden dimensions of kidney disease prognosis.
Crucially, the investigation sheds light on the prognostic significance of an eGFRcys that trails eGFRcr by at least 30%, a threshold that appears not only technically relevant but clinically consequential. In outpatient settings, this substantial gap portends a statistically significant increase in mortality rates, implying that standard creatinine measurements alone may underestimate kidney impairment severity. Such underestimation fosters potential under-recognition of patients at heightened risk for progressive nephropathy and cardiovascular complications.
Delving into inpatient data further underscores the gravity of this marker discordance. The hospitalized cohort, exhibiting a threefold higher prevalence of this discrepancy, reveals the intensified vulnerability of acutely ill individuals. This manifestation may reflect a complex interplay of systemic inflammation, altered protein metabolism, and hemodynamic perturbations characteristic of critical illness, all impacting cystatin C and creatinine metabolism differently and thereby skewing filtration estimations.
The pathophysiological mechanisms underlying the differential clearance and production of cystatin C and creatinine are multifaceted. Cystatin C is freely filtered by glomeruli and almost completely reabsorbed and catabolized by proximal tubular cells without secretion back into the blood, making it a refined marker of glomerular filtration. Conversely, creatinine, while freely filtered, is subject to tubular secretion, especially when renal function declines, potentially masking early kidney dysfunction. This dynamic may account for scenarios wherein cystatin C unearths subclinical renal impairment not readily apparent through creatinine assessment.
From a clinical perspective, recognizing and integrating the discordance between eGFRcys and eGFRcr into patient monitoring protocols could markedly enhance risk stratification. The study advocates for heightened vigilance and possibly supplemental cystatin C testing in individuals with borderline or contradictory creatinine results, thereby refining prognostic accuracy and informing tailored therapeutic interventions. It posits that the eGFRcys-eGFRcr gap could serve as an early alarm for intensified surveillance and preventive care.
Additionally, the findings impel a reevaluation of current kidney disease staging frameworks, predominantly reliant on creatinine-based eGFR. Incorporating cystatin C measurements may redefine staging boundaries and trigger earlier initiation of renoprotective strategies. This paradigm shift could ultimately translate into improved long-term outcomes for at-risk populations by forestalling progression to end-stage renal disease and mitigating cardiovascular morbidity.
Moreover, as cardiovascular events constitute a leading cause of mortality among chronic kidney disease patients, the observed association between eGFR discordance and heightened cardiovascular risk warrants profound attention. The interplay between kidney dysfunction and vascular health is intricate and bidirectional. Biomarker discrepancies might reflect systemic pathological states encompassing endothelial dysfunction, chronic inflammation, and oxidative stress, further compounding cardiovascular vulnerability.
The investigation also opens avenues for novel research exploring biochemical and molecular determinants of cystatin C and creatinine metabolism variations in diverse patient populations. Unraveling these mechanisms holds promise for improving diagnostic algorithms and developing targeted interventions to blunt the impact of kidney disease progression and its systemic sequelae. Future studies could elucidate whether modulating these pathways alters biomarker levels or clinical trajectories.
The implications of this research extend beyond nephrology into broader clinical practice, including hospital medicine and emergency care, where rapid and accurate kidney function assessment critically guides management decisions. Implementing combined biomarker strategies could refine fluid management, medication dosing, and prognostic counseling, thereby mitigating iatrogenic risks and optimizing resource allocation.
Researchers Morgan E. Grams, MD, PhD, and Josef Coresh, MD, PhD, spearhead this study, which represents a significant contribution to the evolving landscape of kidney disease diagnostics and prognostics. Their work, published in the esteemed journal JAMA and unveiled at the American Society of Nephrology Kidney Week 2025 meeting, underscores the dynamic integration of clinical biochemistry and patient-centered outcomes research.
In conclusion, the revelation that a substantial subset of patients exhibit significant discrepancies between cystatin C– and creatinine-based GFR estimates unveils critical vulnerabilities in current kidney disease evaluation practices. The strong association of this discordance with increased mortality, cardiovascular events, and renal failure progression mandates a reassessment of diagnostic protocols. This advancement heralds a precision medicine approach to nephrology, emphasizing biomarker harmonization to optimize patient care and prognosis. As the medical community embraces these insights, transformative enhancements in kidney disease management and patient survival are anticipated.
Subject of Research: Chronic Kidney Disease Prognosis, Biomarker Discrepancy, Kidney Function Assessment
Article Title: Discrepancies Between Cystatin C and Creatinine-Based GFR Estimates Are Linked to Adverse Outcomes in Chronic Kidney Disease
News Publication Date: 2025
References: doi:10.1001/jama.2025.17578
Keywords: Kidney, Mortality rates, Renal failure, Cardiovascular disorders, Hospitals, Patient monitoring, Clinical medicine
Tags: all-cause mortality and kidney functionbiomarkers for renal function assessmentcardiovascular risks and kidney healthchronic kidney disease prognosisclinical outcomes in kidney diseasecreatinine versus cystatin C kidney functionestimated glomerular filtration rate discrepanciesimportance of eGFRcys in clinical practicekidney failure progression and risk factorsmuscle mass impact on creatinine levelsrenal function evaluation methods