Leuven, September 18, 2025 – In a groundbreaking study published in Nature Metabolism, researchers at VIB-KU Leuven Center for Cancer Cell Biology have unveiled a critical mechanism by which melanoma cells dynamically switch between distinctive proliferative and invasive states. This phenotypic plasticity, driven by altered iron metabolism and sophisticated organelle communication, opens new therapeutic avenues to combat tumor progression and drug resistance in one of the deadliest forms of skin cancer.
Melanoma’s notoriety in oncology stems from its aggressive nature and remarkable adaptability. Unlike many cancers that rely solely on genetic mutations to evolve, melanoma cells harness intricate shifts in their internal metabolic landscape to survive therapeutic assaults and colonize distant tissues. Previously, the emphasis had been on genetic and molecular signaling aberrations; however, this study spotlights a subtler but equally vital player: iron trafficking within cancer cells.
At the heart of this cellular ballet lies the reversible transition between two distinct melanoma phenotypes. The melanocytic (MEL) state is characterized by high proliferative capacity and relative susceptibility to contemporary anti-melanoma treatments. Conversely, the mesenchymal-like (MES) state exhibits invasive attributes, enabling cancer cells to metastasize and evade drug-induced death, thereby driving tumor relapse. Understanding how melanoma cells toggle between these states is paramount in overcoming treatment failure and resistance.
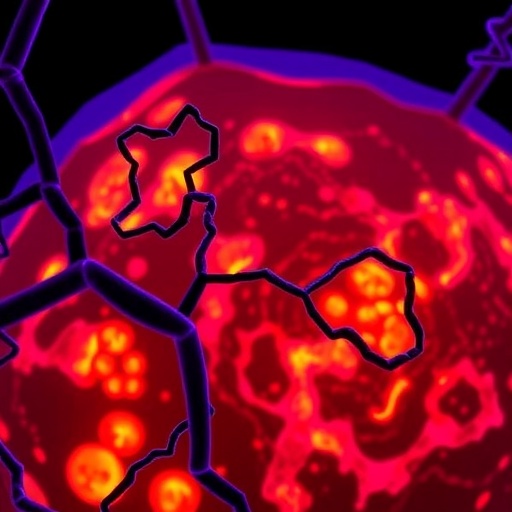
Central to this phenotypic switching is the altered intracellular distribution of iron, pivotal for numerous cellular processes including mitochondrial respiration and enzymatic reactions. The study unveils a disruption in iron transport between mitochondria and lysosomes—organelles that serve as iron repositories and regulators of cellular iron homeostasis. This disturbance is orchestrated through modulation of a single enzyme, BDH2, which emerges as a linchpin in iron trafficking machinery.
BDH2, an enzyme traditionally recognized for its role in metabolic pathways, synthesizes a small molecule siderophore that binds and shuttles iron into mitochondria. The research reveals that downregulation of BDH2 in melanoma cells precipitates iron accumulation within lysosomes, facilitating the MES phenotype’s invasive capabilities. Intriguingly, this phenomenon mirrors bacterial survival strategies, where similar siderophore systems procure iron essential for growth, underscoring an evolutionary conservation of iron transport pathways.
The consequences of disrupted BDH2 activity extend beyond mere iron localization. MES cells experiencing lysosomal iron overload become exquisitely vulnerable to ferroptosis, an iron-dependent form of regulated cell death marked by lipid peroxidation and oxidative damage. This vulnerability presents a paradox: while MES cells evade conventional therapies, their iron-mediated susceptibility to ferroptosis could be exploited therapeutically to eradicate drug-resistant populations.
Experimental restoration of BDH2 expression recalibrates iron transport, bolstering mitochondrial function and normalizing iron homeostasis. This reestablishment reduces MES cells’ susceptibility to ferroptosis, particularly critical during hematogenous dissemination, where circulating tumor cells endure oxidative stress. Thus, BDH2 functions not only in metabolic regulation but also in dictating melanoma cell fate under hostile microenvironmental conditions.
Prof. Patrizia Agostinis, leading the investigative team, emphasizes that these insights reveal an uncharted layer of metabolic regulation linking organelle crosstalk to cancer cell plasticity and survival. By targeting components of iron homeostasis and the molecular mediators facilitating lysosome-mitochondria iron transfer, novel strategies could emerge to curtail tumor progression and overcome resistance mechanisms that undermine current therapies.
From a biochemical standpoint, this study integrates meticulous experimental approaches, including molecular biology techniques, metabolic flux analysis, and ferroptosis assays, to dissect the nuances of iron metabolism in melanoma. The identification of BDH2 as a regulatory node offers a tangible target for drug development and biomarker discovery, enabling precision oncology approaches tailored to tumor metabolic states.
Moreover, the findings raise the prospect that similar iron trafficking perturbations might underlie phenotypic plasticity in other malignancies exhibiting metabolic flexibility and therapy tolerance. This expands the impact of the work beyond melanoma and sets the stage for broader investigations into iron metabolism as a universal determinant of cancer aggressiveness.
Importantly, this research underscores the complexity of tumor biology, where organelle interaction and metabolic adaptation converge to dictate cell behavior. The lysosome and mitochondrion, often studied in isolation, are revealed here as cooperative partners orchestrating a critical survival axis via iron transfer, fundamentally influencing cell fate decisions in the context of cancer.
As the oncology field strives to develop therapies that preempt resistance and eradicate minimal residual disease, leveraging ferroptosis through manipulation of iron metabolism emerges as a promising frontier. The vulnerabilities exposed by BDH2 dysregulation and iron misallocation highlight a metabolic Achilles’ heel in aggressive melanoma cells.
With cancer mortality rates remaining stubbornly high, especially due to metastatic disease, the elucidation of such intricate intracellular pathways offers hope for transformative treatment paradigms. Future therapeutic approaches may harness the delicate balance of iron-mediated metabolic states to selectively induce ferroptosis in invasive melanoma cells, sparing normal tissue and minimizing side effects.
In conclusion, the VIB-KU Leuven study provides compelling evidence that metabolic regulation through iron trafficking and organelle crosstalk shapes melanoma cell phenotypic plasticity and vulnerability to cell death. This refined understanding not only advances fundamental cancer biology but also paves the way for innovative, metabolism-focused therapeutic interventions poised to change the landscape of melanoma treatment.
Subject of Research: Animals
Article Title: BDH2-driven lysosome-to-mitochondria iron transfer shapes ferroptosis vulnerability of the melanoma cell states
News Publication Date: 18-Sep-2025
Web References: 10.1038/s42255-025-01352-4
Keywords: Diseases and disorders, Clinical medicine, Health care, Immunology
Tags: dynamic adaptation of melanoma cellsgenetic mutations in melanomainvasive melanoma characteristicsiron metabolism in melanomamelanoma cell states comparisonmelanoma phenotypic plasticitymetastatic behavior of melanomaNature Metabolism study on melanomaorganelle communication in cancer cellstherapeutic strategies for melanomatumor progression and drug resistanceVIB-KU Leuven cancer research