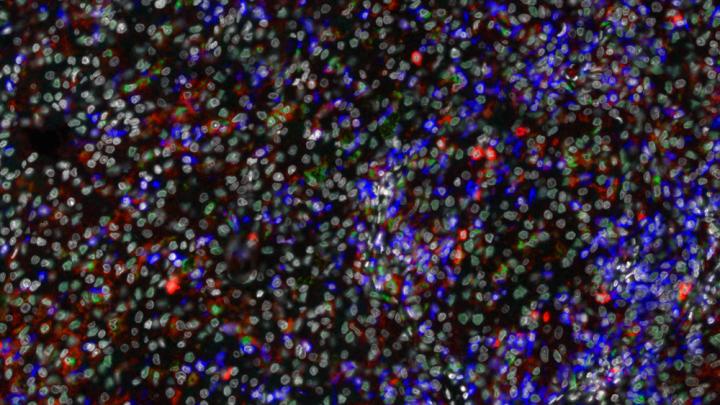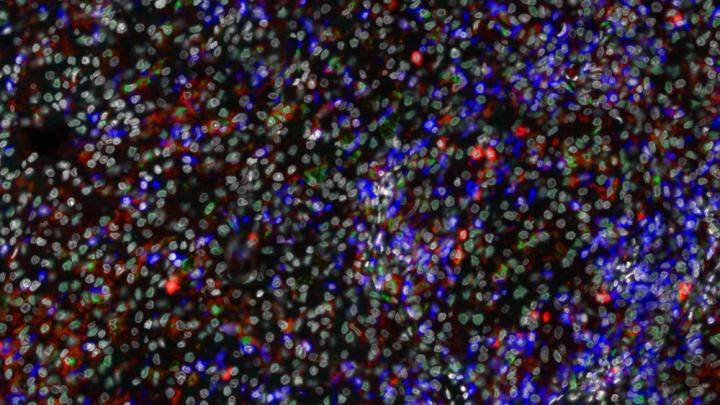
Credit: Karina Silina, University of Zurich
Renal cell carcinoma is one of the most frequent and deadly urogenital cancers. Even if the tumors are treated, they ultimately end in metastasis in about half of the patients. 90 percent of these patients die within five years. Thanks to new kinds of immunotherapies, the outlook of this patient group has improved, but the treatment only works for a minority of patients.
Composition of immune cells influences the prognosis of patients
To find out more about the body`s own defense against cancer cells – and how it can be strengthened – researchers headed by Bernd Bodenmiller at the Institute of Molecular Life Sciences of the University of Zurich have individually analyzed a total of 3.5 million immune cells in the tumor samples of 73 patients with renal cell carcinoma and in five healthy controls. "The previous picture of immune defense was correct, but coarse," says first author of the study, Stéphane Chevrier. "With our methods to analyze individual immune cells, we have been able to create an immunological atlas of the tumor environment for the first time with high resolution and in a large patient cohort. As a result, many more facets have now come to light."
Whether a tumor can develop and persist at a certain point in the body mainly depends on the response of the immune system in the direct vicinity of the tumor. As the scientists report in the journal Cell, they have identified new relationships between the various immune cells thanks to the immune atlas. In particular, the researchers have defined so-called immune cell signatures connected to the prognosis of the patients. The type and number of protein structures on the surface of immune cells play an essential role in regard to how the disease proceeds and how a patient responds to immunotherapies. "Such information can help us better understand how these treatments can be adapted individually within the scope of personalized medicine," Bernd Bodenmiller concludes.
Interruption of an additional signalling pathway as possible therapeutic objective
In addition, Bodenmiller's team has shown that certain surface molecules with a therapeutic use (so-called checkpoints, such as PD-1 or CTLA-4) cannot be found on the immune cells of all patients. Substances that block these surface proteins prevent the immune cells from being inactivated during the defense against cancer. These results could explain why the new types of checkpoint inhibitors work only for a minority of patients. With complex bioinformatic analyses, the group also discovered an additional target molecule called CD38, which can be found on the surface of inactivated or exhausted T-cells. Whether more renal cell carcinoma patients could be helped by targeting this additional CD38 signalling pathway will become clear in the near future. Bodenmiller's research partners in Australia have already started to plan corresponding clinical testing.
###
Media Contact
Bernd Bodenmiller
[email protected]
41-446-353-128
@uzh_news
http://www.uzh.ch
############
Story Source: Materials provided by Scienmag