In a groundbreaking study set to redefine our understanding of neuroprotection, researchers have uncovered a compelling molecular mechanism by which carbon monoxide (CO) exerts a protective effect on neuronal cells. This latest research, led by Park, Jin, Song, and colleagues, elucidates how CO activates the PERK-calcineurin signaling axis, ultimately curbing necroptosis—a form of programmed necrotic cell death that has been implicated in neurodegenerative diseases. Their findings, published in the highly regarded journal Cell Death Discovery, open a promising therapeutic avenue against a spectrum of neurological disorders characterized by neuronal loss and inflammation.
Traditionally known as a toxic gas, carbon monoxide’s role in biology has been paradoxical and enigmatic. While high concentrations of CO are lethal, emerging evidence over the last decade has revealed that at low, controlled doses, CO functions as a gaseous neurotransmitter and modulates diverse cellular processes. In this new research, the investigators sought to unravel how CO could serve as a neuroprotective agent, especially in the context of necroptosis, a form of regulated cell death distinct from apoptosis and central to neuroinflammation and neurodegeneration.
Central to their discovery is the identification of the PERK (PKR-like endoplasmic reticulum kinase) pathway as a key mediator of CO’s protective effects. PERK, a sensor of endoplasmic reticulum (ER) stress, is known to initiate adaptive responses critical for cell survival under adverse conditions. The research team showed that CO activates PERK in neuronal cells, setting off a cascade that engages calcineurin, a calcium/calmodulin-dependent phosphatase previously recognized for its roles in synaptic plasticity and immune regulation.
Through a combination of cutting-edge biochemical assays, live-cell imaging, and genetically engineered neuronal models, the team meticulously mapped the biochemical sequence from CO exposure to PERK activation and subsequent calcineurin-mediated suppression of necroptotic effectors. This required dissecting the interaction of key proteins such as RIPK3 and MLKL, which comprise the necrosome complex—the critical mediator of necroptotic cell death.
The implications of this discovery extend beyond neuroprotection. Considering the ubiquitous presence of necroptosis in various pathological contexts, the ability to modulate this death pathway with a small, diffusible molecule like CO offers a versatile platform for therapeutic development. The researchers anticipate that harnessing CO’s properties, either through CO donors or modulators of the PERK-calcineurin pathway, could lead to innovative treatments not only for neurodegenerative diseases but also for acute neuronal injuries such as stroke and traumatic brain injury.
However, the authors caution that translational hurdles remain. Given CO’s toxicity at elevated levels, establishing safe therapeutic windows and delivery mechanisms will be paramount. The study calls for further in vivo validation using animal models to explore dosing regimens, distribution, and long-term effects of CO-based interventions. Such preclinical studies will be critical to ensure effective neuroprotection without adverse systemic toxicity.
Intriguingly, the study also sheds light on how cellular stress responses can be harnessed therapeutically. PERK is typically activated under ER stress conditions to restore homeostasis. Here, CO appears to mimic or potentiate this natural protective mechanism. This insight aligns with emerging paradigms in cell biology that emphasize modulating stress pathways for disease intervention instead of merely inhibiting pathological processes.
Moreover, this research underscores the versatility of gaseous signaling molecules in biology. Alongside nitric oxide and hydrogen sulfide, CO is now firmly recognized as a bioactive gasotransmitter. The controlled manipulation of these gaseous messengers represents a fertile area for drug discovery, offering spatially and temporally precise modulation of intracellular pathways.
At a molecular level, the interplay between PERK and calcineurin adds a new dimension to the regulatory networks governing neuronal survival and death. Calcineurin’s dephosphorylation activity influences numerous substrates, including nuclear factor of activated T-cells (NFAT) transcription factors, which could integrate signals from CO exposure to guide gene expression changes relevant to neuroprotection. Deciphering these downstream effectors represents a tantalizing frontier for future research.
Furthermore, this study’s approach integrates multidisciplinary techniques bridging molecular biology, neurochemistry, and pharmacology. The use of genetically encoded reporters to monitor necroptosis dynamics allowed the team to observe real-time effects of CO at a cellular level. Combining such tools with transcriptomics or proteomics could further highlight global cellular changes orchestrated by CO-driven PERK-calcineurin signaling.
From a clinical standpoint, this work resonates with the urgent need for novel neuroprotective strategies. Existing treatments for neurodegenerative disorders are largely symptomatic and fail to halt or reverse neuronal loss. Targeting necroptosis offers a distinct mechanism to preserve neuronal integrity and reduce harmful inflammation. CO’s dual role in modulating stress responses and inhibiting necroptosis makes it uniquely suited to this purpose.
In summary, Park, Jin, Song, and colleagues’ seminal study revolutionizes our understanding of CO as a neuroprotective agent. By mapping the detailed molecular crosstalk between CO, PERK activation, calcineurin signaling, and necroptosis inhibition, it provides a robust framework for next-generation therapeutic concepts. The research highlights the remarkable potential of physiologically relevant gases to fine-tune critical survival pathways in neurons, ultimately fostering resilience against degenerative insults.
As interest in gaseous signaling continues to surge, this study positions CO-based interventions at the forefront of neurotherapeutics. With continued research, translating these insights into clinical reality could offer hope to millions affected by debilitating neurological diseases worldwide. The promise of harnessing a traditionally feared molecule like CO to preserve brain health exemplifies the power of innovative science to transform challenges into cures.
Subject of Research: Neuroprotection via carbon monoxide-mediated activation of the PERK-calcineurin pathway and inhibition of necroptosis.
Article Title: CO confers neuroprotection via activating the PERK-calcineurin pathway and inhibiting necroptosis.
Article References:
Park, J., Jin, L., Song, HC. et al. CO confers neuroprotection via activating the PERK-calcineurin pathway and inhibiting necroptosis. Cell Death Discov. 11, 254 (2025). https://doi.org/10.1038/s41420-025-02530-9
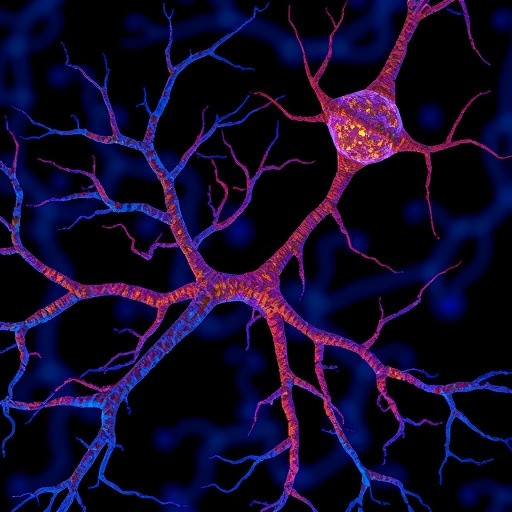
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02530-9
Tags: carbon monoxide neuroprotectiongaseous neurotransmitter functionslow-dose carbon monoxide therapymolecular mechanisms of COnecroptosis in neurodegenerationneuroinflammation and neuroprotectionneuronal cell death mechanismsneuroprotective agents in researchPERK pathway activationprogrammed cell death in neuronssignaling pathways in neurobiologytherapeutic approaches for neurological disorders