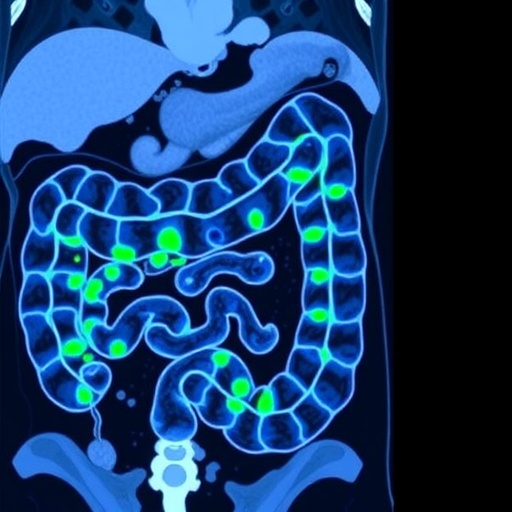
In a groundbreaking study poised to transform colorectal cancer screening, researchers have harnessed the power of Optical Coherence Tomography (OCT) to distinguish between benign and potentially malignant colon polyps with unprecedented accuracy. This innovative application of OCT imaging offers a promising pathway toward more targeted, less invasive strategies in colorectal cancer management, particularly through the “leave-in-situ” approach for diminutive polyps.
Colorectal cancer remains a leading cause of cancer-related mortality worldwide, with early detection and removal of malignant or pre-malignant polyps being crucial to improving patient outcomes. However, prevailing clinical protocols often necessitate the excision of even small polyps, leading to unnecessary procedures with associated risks and healthcare costs. The recent study by Photiou et al. delves into the realm of advanced imaging analysis to refine the diagnostic precision required for safely leaving certain diminutive polyps undisturbed.
At the core of this research is the utilization of Optical Coherence Tomography, an imaging modality capable of producing high-resolution, cross-sectional views of tissue microstructures without the need for invasive biopsies. By applying OCT to resected colon polyps ex vivo, the team extracted a comprehensive array of features that act as biomarkers to characterize the tissue’s pathological state. Unlike traditional imaging methods reliant primarily on intensity measurements, this study integrates novel parameters such as scatterer size, group velocity dispersion, and spectral data, enriching the diagnostic dataset.
The statistical analysis of these diverse OCT-derived features has led to the development of robust classification algorithms capable of differentiating benign polyps—such as normal mucosa and hyperplastic polyps—from those harboring malignant potential, including adenomas and sessile serrated adenomas. This distinction is critical because only the latter category necessitates immediate removal due to their propensity to progress to cancer.
One of the most compelling findings of the study is the exceptional accuracy achieved when classifying whole polyp sections by integrating multiple feature scores. This multifaceted approach attained a remarkable 97.3% accuracy and a 95.5% negative predictive value, indicating a high level of confidence in ruling out malignancy in identified benign polyps. Even when assessing individual OCT images, the methodology yielded an accuracy close to 80%, underscoring the potential clinical utility of this technology in real-time decision-making scenarios.
The implications for clinical practice are profound. Implementing OCT-based classification during colonoscopic procedures could drastically reduce unnecessary polypectomies for diminutive polyps that pose minimal risk, thereby decreasing patient burden and healthcare expenditures. This aligns with the Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI-1) criteria, which emphasize enhanced diagnostic performance as a prerequisite for adopting leave-in-situ strategies.
Technically, the success of the study hinges on the sophisticated feature extraction pipeline designed to capture subtle variations in tissue optical properties. Scatterer size, for instance, correlates with cellular and subcellular structures, providing insight into morphological alterations linked to neoplastic progression. Meanwhile, group velocity dispersion reflects the dispersive characteristics of tissue, offering additional contrast between normal and abnormal histology. The spectral analysis further complements these features by dissecting the wavelength-dependent properties of the backscattered light.
The approach moves beyond mere image interpretation; it applies advanced statistical frameworks to synthesize multidimensional data into clinically actionable scores. These composite scores enable a probabilistic classification that balances sensitivity and specificity, tailoring the diagnostic threshold according to clinical requirements. Such data-driven rigor ensures that false negatives—critical in cancer detection—are minimized without compromising the detection of benign lesions.
Future directions for this research encompass validation in in vivo settings during real-time colonoscopy, integration with endoscopic equipment, and exploration of machine learning algorithms to automate classification further. The seamless translation of this technology into everyday clinical workflows could revolutionize colorectal cancer screening protocols, enabling personalized surveillance and minimizing overtreatment.
Additionally, this study exemplifies the broader trend of leveraging optical imaging and computational analytics to enhance cancer diagnostics. The ability to non-invasively probe tissue microarchitecture at high resolution offers a versatile platform applicable across various oncological domains, heralding a new era of precision medicine grounded in biophysical characterization.
In summary, the pioneering work by Photiou and colleagues demonstrates that the marriage between Optical Coherence Tomography and sophisticated statistical analysis holds tremendous promise for the future of colorectal cancer prevention. By enabling accurate discrimination of polyps with malignant potential, this approach paves the way for safer, more efficient screening strategies that could significantly reduce patient morbidity and healthcare costs worldwide.
Subject of Research: Optical Coherence Tomography-based classification of colorectal polyps to determine malignant potential.
Article Title: Classification of colon polyps with malignant potential using statistical analysis of features extracted from ex vivo optical coherence tomography images.
Article References:
Photiou, C., Thrapp, A.D., Tearney, G.J. et al. Classification of colon polyps with malignant potential using statistical analysis of features extracted from ex vivo optical coherence tomography images. BioMed Eng OnLine 24, 108 (2025). https://doi.org/10.1186/s12938-025-01443-z
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12938-025-01443-z
Tags: advanced diagnostic methods for polypscolorectal cancer mortality reduction strategiesearly detection of colorectal cancerex vivo analysis of colon polypsimaging biomarkers for tissue characterizationinnovative imaging techniques for polypsleave-in-situ approach for diminutive polypsmalignant colon polyp classificationnon-invasive colorectal cancer screeningOCT imaging in cancer managementOptical Coherence Tomography in colorectal cancerreducing unnecessary polyp excisions