With the aging of the global population, the prevalence of metabolic diseases has significantly increased over the past two decades. Meanwhile, China grapples with the largest population aged 65 years and older and a faster pace of population aging than many other countries. This demographic shift contributes to the escalating burden of age-related chronic diseases. Accumulating evidence also suggests gender disparities in the prevalence and incidence of chronic diseases, and while numerous studies have been conducted on this topic, many overlook the crucial covariate of age.
With the aging of the global population, the prevalence of metabolic diseases has significantly increased over the past two decades. Meanwhile, China grapples with the largest population aged 65 years and older and a faster pace of population aging than many other countries. This demographic shift contributes to the escalating burden of age-related chronic diseases. Accumulating evidence also suggests gender disparities in the prevalence and incidence of chronic diseases, and while numerous studies have been conducted on this topic, many overlook the crucial covariate of age.
Recognizing the interplay between sex and age is crucial for understanding the trajectories of cardiometabolic diseases and its upstream risk factors, as well as for promoting individualized intervention strategies. Previous studies in the global or European population investigated the age-related sex differences in a range of risk factors, but there is a paucity of gender-specific analyses pertaining to the trajectories of risk factors for adults in China.
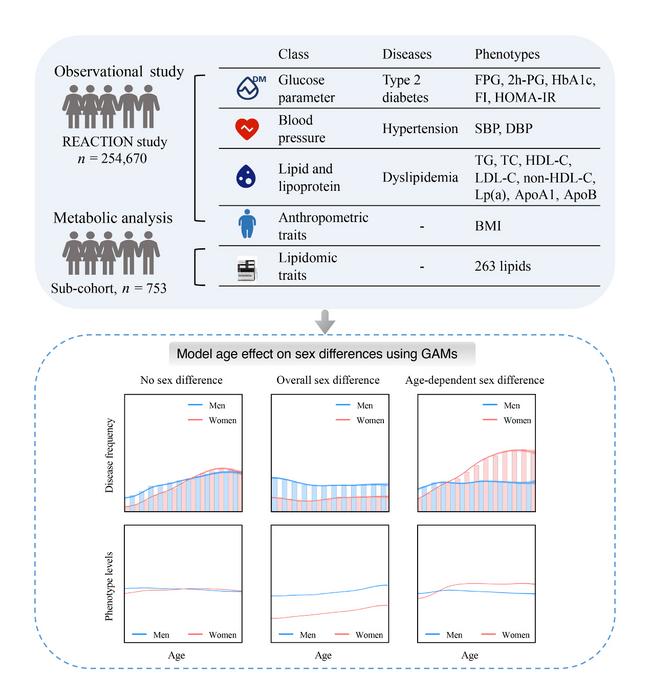
Recently, Dr. Weiqing Wang at Ruijin Hospital affiliated with Shanghai Jiao Tong University School of Medicine published a paper in Life Metabolism entitled “Exploring age and gender disparities in cardiometabolic phenotypes and lipidomic signatures among Chinese adults: a nationwide cohort study”. Based on the Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal (REACTION) study, a total of 254,670 adults aged 40−80 years were included in this study, who were recruited from 25 local centers across mainland China.
The study employed a range of analytical methods to investigate the dynamic impact of age and gender on metabolic risk factors and lipid profiles associated with cardiovascular disease (Figure 1). Firstly, regression analysis was used to evaluate the differences in metabolic disease risks, particularly dyslipidemia and its components, between females and males across various age groups. Secondly, generalized additive models were applied to elucidate the trends in gender differences in modifiable metabolic risk factors over time. The results indicated that these gender differences were not static but exhibited significant interactions with age. Three distinct patterns were observed: minor sex differences, pronounced sex differences, and significant age-gender interactions in four lipid indicators. Thirdly, the sliding window t-test method was employed to identify the inflection points where lipid indicators shifted with age. This approach helped pinpoint specific age ranges where gender differences became more pronounced. Additionally, the study found a three-way interaction between sleep duration, age, and gender affecting lipid levels. This finding underscores the complex modulation of lipid levels by both age and gender, influenced by sleep duration. Furthermore, the contribution of gender, age, and their interaction to the variance in various lipidomic traits was quantified. K-means clustering was used to explore the impact of these factors on serum lipidomic profile, leading to the classification of lipoproteins based on gender and age.
In conclusion, the study demonstrates that gender differences in cardiovascular metabolic disease risk, cholesterol, triglyceride levels, and lipid metabolic profiles are not fixed but interact significantly with age. Ignoring age-related variations may obscure true gender effects or lead to erroneous conclusions. The findings highlight the importance of considering age in studies of gender differences in metabolic diseases and advocate for personalized prevention and management strategies tailored to different age groups.
Journal
Life Metabolism
DOI
10.1093/lifemeta/loae032
Method of Research
Observational study
Subject of Research
People
Article Title
Exploring age and gender disparities in cardiometabolic phenotypes and lipidomic signatures among Chinese adults: a nationwide cohort study
Article Publication Date
2-Aug-2024