Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects millions of women worldwide. Despite its prevalence, many aspects of PCOS remain poorly understood, prompting ongoing research to uncover effective treatment options. A groundbreaking study conducted by Yang et al. has shed light on the effects of two common medications—chiglitazar and metformin—on insulin resistance, particularly among women with a normal Body Mass Index (BMI) diagnosed with PCOS. These findings open new avenues for managing this multifaceted condition that impacts not only reproductive health but also metabolic function.
Insulin resistance is a well-known feature of PCOS and is believed to be a contributing factor to the disorder’s symptoms and complications. Women with PCOS typically exhibit higher insulin levels, which can lead to weight gain, fertility issues, and an increased risk of developing type 2 diabetes. Metformin, a medication commonly prescribed to manage insulin levels in people with type 2 diabetes, has been a staple in treating PCOS. However, the introduction of chiglitazar—a novel drug with a unique mechanism—raises questions about its comparative effectiveness against metformin.
The study by Yang et al. is significant in that it targets not just women with PCOS who are overweight or obese, but those within the normal BMI range. This is particularly relevant since traditional approaches to PCOS management have often overlooked this demographic. By focusing on women with normal BMI, the research addresses a critical gap in understanding how insulin resistance manifests across different body types and how treatment efficacy may vary accordingly.
The randomized controlled trial methodology employed by Yang and colleagues provides a robust framework for evaluating the relative effects of both medications. Participants were meticulously selected, ensuring that they met specific criteria that align with the study’s objective. Through random assignment to either the chiglitazar or metformin group, the researchers aimed for a balanced comparison, thereby minimizing bias and confounding variables.
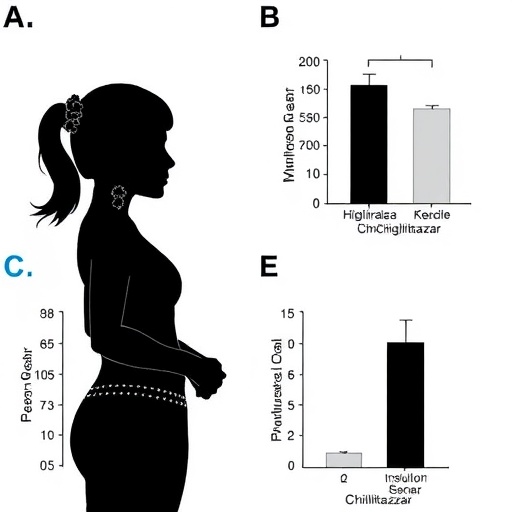
A total of 200 women participated in the study, each diagnosed with PCOS and exhibiting symptoms characteristic of the condition. Each group received either chiglitazar or metformin for a period of 12 weeks, during which they underwent regular assessments of their insulin sensitivity through standardized tests. Key measurements included fasting insulin levels, glucose tolerance, and various hormonal profiles to evaluate the overall metabolic impact of each treatment.
Results from the study revealed that chiglitazar significantly improved insulin sensitivity in participants when compared to metformin. While both medications had positive effects, chiglitazar’s impact was observed to be more pronounced, especially in terms of reducing insulin levels and improving glucose metabolism. This finding may lead to a reevaluation of treatment protocols for PCOS, particularly for those women whose insulin resistance does not respond adequately to metformin.
The implications of these findings extend beyond just managing PCOS symptoms. Improved insulin sensitivity can lead to better metabolic health, significantly reducing the risk of long-term complications such as diabetes and cardiovascular disease. By addressing insulin resistance effectively, women with PCOS may experience a broader range of health benefits that contribute to their overall well-being and quality of life.
Furthermore, the study’s insights can influence clinical practice and policy decisions concerning women’s health. If chiglitazar proves to be a superior option for managing insulin resistance in normal-weight women, it could prompt healthcare providers to adopt this approach more widely, thus tailoring treatment plans to better suit individual patient profiles. This could also stimulate further research into additional therapeutic options that can address the underlying causes of insulin resistance in various populations.
Moreover, patient education plays a crucial role in the management of PCOS. The study underscores the importance of healthcare professionals being equipped with the latest research findings to advise their patients effectively. Many women with PCOS remain unaware of the potential risks associated with insulin resistance and the available treatment options. The dissemination of this information can empower patients to take an active role in their health, enhancing adherence to treatment regimens and lifestyle modifications.
In conclusion, the findings from Yang et al. offer a promising perspective on treating insulin resistance in women with PCOS. By highlighting the comparative effects of chiglitazar and metformin, the research may catalyze a shift in clinical practice and enhance the quality of life for countless women affected by this disorder. As the medical community continues to explore the complexities of PCOS, studies like this pave the way for more effective, personalized strategies that can address the unique challenges faced by those with this condition.
The continuous exploration of novel treatments like chiglitazar will ultimately contribute to a more nuanced understanding of PCOS and its management. Future research should aim to replicate these findings across more diverse populations and to investigate the long-term effects of these medications on metabolic health and reproductive outcomes.
As awareness surrounding PCOS grows, the need for innovative treatments becomes increasingly crucial. The study’s promising results with chiglitazar not only provide hope for women with PCOS but also encourage ongoing efforts to improve our collective understanding of this multifaceted syndrome. With further advancements in research and treatment options, there is potential for a future where the burden of PCOS can be significantly alleviated, leading to healthier outcomes for women everywhere.
Subject of Research: The effects of chiglitazar and metformin on insulin resistance in women with a normal BMI and polycystic ovary syndrome.
Article Title: The effects of chiglitazar and metformin on insulin resistance in women with a normal BMI and polycystic ovary syndrome: a randomized controlled study.
Article References: Yang, Y., Han, Y., Xu, J. et al. The effects of chiglitazar and metformin on insulin resistance in women with a normal BMI and polycystic ovary syndrome: a randomized controlled study. BMC Endocr Disord (2025). https://doi.org/10.1186/s12902-025-02082-0
Image Credits: AI Generated
DOI: Not available.
Keywords: Polycystic Ovary Syndrome, insulin resistance, chiglitazar, metformin, randomized controlled trial, women’s health.
Tags: Chiglitazar for insulin sensitivitydiabetes risk in PCOS patientseffective medications for insulin resistancehormonal disorders and PCOSinsulin resistance in womenmanaging PCOS symptomsmetabolic function in PCOSMetformin and PCOS treatmentnormal BMI PCOS managementnovel treatments for PCOSreproductive health and insulinYang et al. PCOS study