Chemotherapy is a commonly used regimen for cancer treatment, but it is also a double-edged sword. While the drugs are highly effective at killing cancer cells, they are also notorious for killing healthy cells in the body. As such, minimizing the drug’s damage to the patient’s body is necessary to improve the prognosis of chemotherapy.
Credit: Institute for Basic Science
Chemotherapy is a commonly used regimen for cancer treatment, but it is also a double-edged sword. While the drugs are highly effective at killing cancer cells, they are also notorious for killing healthy cells in the body. As such, minimizing the drug’s damage to the patient’s body is necessary to improve the prognosis of chemotherapy.
Recently, “chronochemotherapy” have been gaining key interest in the research community. As the name suggests, the aim is timing the delivery of the drug when the body is least vulnerable to the harmful effects of the drug, while the cancer cells are at their most vulnerable.
Chronochemotherapy exploits the fact that human physiological processes, including cell proliferation and differentiation, are regulated by an endogenous timer called the circadian clock. However, it is not yet widely exploited in real-world clinical settings because as of now, there is no systematic method to find the optimal chemotherapy delivery time.
This problem was tackled by an interdisciplinary team of researchers from South Korea. They were led by the principal investigators KIM Jae Kyoung (a mathematician at Biomedical Mathematics Group, Institute for Basic Science) and KOH Youngil (an oncologist at Seoul National University Hospital). The researchers studied a group of patients suffering from Diffuse large B-cell lymphoma (DLBCL).
Terminology
* Diffuse large B-cell lymphoma (DLBCL): Lymphoma is a type of blood cancer caused by the malignant transformation of lymphoid tissue cells. Lymphoma is divided into Hodgkin’s lymphoma and non-Hodgkin’s lymphoma (malignant lymphoma), and diffuse large B-cell lymphoma accounts for about 30 to 40% of non-Hodgkin’s lymphoma.
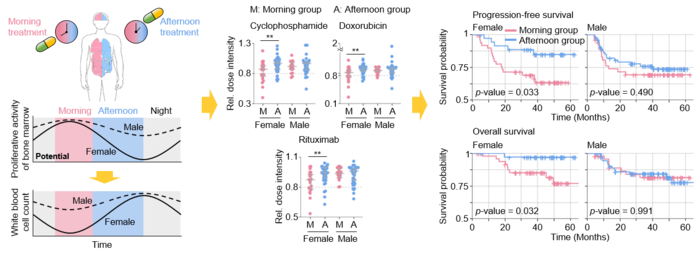
The research team noticed that DLBCL patients at Seoul National University Hospital received chemotherapy at two different schedules, with some patients receiving morning treatment (8:30 a.m.), while others taking the drugs in the afternoon (2:30 p.m.). All patients received the same cancer treatment (R-CHOP), which is a combination of targeted therapy and chemotherapy, 4 to 6 times in the morning or afternoon at intervals of about 3 weeks.
They analyzed 210 patients to investigate whether there is any difference between morning and afternoon treatment. It was found that female patients who received afternoon treatment had 12.5 times reduced mortality rate (25% to 2%), while the cancer recurrence after 60 months was decreased by 2.8 times (37% to 13%). In addition, chemotherapy side effects such as neutropenia were more common in female patients who received morning treatment.
Surprisingly, there was no difference in treatment efficiency depending on the treatment schedule in the case of male patients.
To understand the cause of gender differences, the research team analyzed ~14,000 blood samples from the Seoul National University Hospital Health Examination Center. It was found that in females, white blood cell count tends to decrease in the morning and increase in the afternoon. This indicates that the bone marrow proliferation rate is higher in the morning than in the afternoon because there is a ~12hr delay between the bone marrow proliferation and blood cell production.
This means that if a female patient receives chemotherapy in the morning when bone marrow is actively producing blood cells, the possibility of adverse side effects becomes greater. These results are consistent with the findings from recent randomized clinical trials that showed female colorectal cancer patients treated with irinotecan in the morning suffered from higher drug toxicities.
One confounding variable was the drug dose. Since the morning female patients suffered from greater adverse side effects, oftentimes the dose had to be reduced in these patients. On average, the drug dose was reduced by ~10% compared to the dose intensity given to female patients receiving the afternoon treatment.
Unlike female patients, it was found that male patients did not show a significant difference in white blood cell count and bone marrow cell proliferation activity throughout the day, which is the reason why the timing of the treatment had no impact.
Professor KOH Young-il said, “We plan to verify the conclusions of this study again with a large-scale follow-up study that completely controls confounding variables, and to confirm whether chemotherapy has similar effects in other cancers.”
CI KIM Jae Kyung said, “Because the time of the internal circadian clock can vary greatly depending on the individual’s sleep-wake patterns, we are currently developing a technology to estimate the time of the circadian clock from the patient’s sleep pattern. We hope that it can be used to develop an individualized anti-cancer chronotherapy.”
Journal
JCI Insight
DOI
10.1172/jci.insight.164767
Method of Research
Randomized controlled/clinical trial
Subject of Research
People
Article Title
Chemotherpay delivery time affects treatment outcomes of female patients with diffuse large B-cell lymphoma
Article Publication Date
13-Dec-2022




