Credit: Journal of the American Osteopathic Association
CHICAGO–January 11, 2018–Physicians determining treatment options following abnormal Pap smears now have another factor to consider: the patient's race.
According to new research in The Journal of the American Osteopathic Association, the rates at which precancerous cells in the cervix progress toward becoming cancerous or regress toward normal vary among Hispanic, black, white, and Asian women.
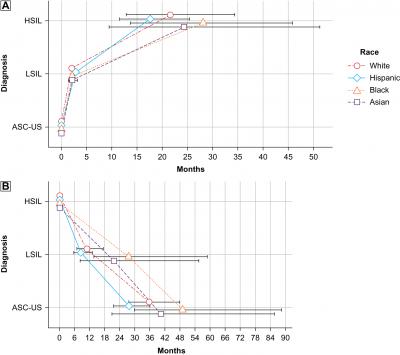
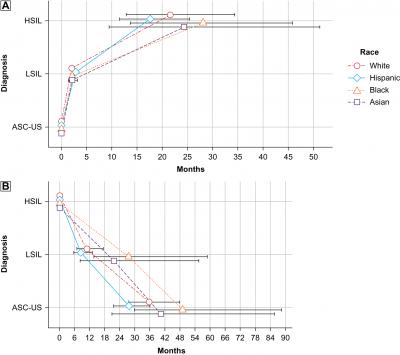
The study analyzed medical records of 5472 women receiving a Pap test between January 2006 and September 2016, and charted the progression of abnormal cell development, from the atypical but innocuous (ASC-US) lesions to low-grade (LSIL) to high-grade (HSIL), the type most likely to develop into cancer. Researchers also studied the rates at which lesions regressed from HSIL to ASC-US stage.
"We see race-based differences that influence treatment protocols in all manner of health issues," said Daniel Martingano, DO, an OB/GYN at New York University Langone Hospital–Brooklyn and lead author on this study. "Unfortunately, screening and treatment guidelines for precancerous lesions have not yet benefited from that additional layer of context. This study is a first step toward more precise and effective care."
Hispanic women progressed the fastest, moving from innocuous to worrisome high-grade lesions within 17.6 months, whereas black women took 27.6 months to reach that critical state. However, Hispanic women recovered faster too, regressing from high-grade to innocuous lesions in 28.1 months. On average black women took 49 months to regress back to the innocuous stage.
Progression and regression rates of precancerous lesions for white and Asian women fell in between, reflecting more closely the expected patterns upon which current treatment guidelines are based.
Dr. Martingano says his research may help physicians feel more confident in making their treatment decisions and hopes it leads to fewer women undergoing aggressive and invasive procedures.
Tipping the scales in risk assessment
Precancerous lesions are caused by the human papillomaviruses (HPV) and can lead to cervical cancer. Often the immune system is able to fight off the virus, and when it does, precancerous lesions tend to regress back to normal cells.
This is why, when precancerous lesions are discovered, the next step is usually to test for HPV. Physicians determine their recommendation for treatment by calculating risk, which depends on the stage of the lesion and whether HPV is still present.
Aggressive treatment usually involves excising the lesion. While this effectively eliminates the risk for developing cancer, it also compromises the cervix and can negatively affect reproductive health–especially if the procedure is done multiple times over a patient's life.
Tailored treatment
"Precancerous lesions in black women seem to take a significantly longer time to progress to a dangerous level," said Dr. Martingano. "In cases of abnormal cells and low grade lesions, we have a lot more latitude to give their bodies time to fight the virus and recover on their own."
Conversely, he says Hispanic women who have low grade lesions and test positive for HPV should probably be treated more aggressively as they worsen the fastest.
"We know different groups of people follow different trajectories in relation to disease progression," said Dr. Martingano. "Whenever we are able to tailor our treatment accordingly, it's always the most beneficial approach for our patients."
###
About The Journal of the American Osteopathic Association
The Journal of the American Osteopathic Association (JAOA) is the official scientific publication of the American Osteopathic Association. Edited by Robert Orenstein, DO, it is the premier scholarly peer-reviewed publication of the osteopathic medical profession. The JAOA's mission is to advance medicine through the publication of peer-reviewed osteopathic research.
Media Contact
Jeff Brennan
Media Relations Manager
312-202-8161
[email protected]
Media Contact
Jeff Brennan
[email protected]
312-202-8161
@aoafordos
Original Source
http://jaoa.org/article.aspx?articleid=2668393 http://dx.doi.org/10.7556/jaoa.2018.003