In the relentless quest to overturn the biological complexities of cancer, a recent breakthrough sheds new light on the insidious phenomenon of cancer cachexia, particularly within the context of STK11/LKB1-mutated non-small cell lung cancer (NSCLC). Published in Nature Communications, the study by Yu, Guo, Gupta, and colleagues uncovers a pivotal role for tumor-secreted growth differentiation factor 15 (GDF15) as a key driver of this wasting syndrome. This discovery not only deepens our understanding of tumor-host interactions but also opens promising avenues for targeted therapeutic intervention against cancer-induced cachexia.
Cancer cachexia—a multifaceted syndrome characterized by severe body weight, muscle, and fat loss—is a devastating condition that afflicts a substantial subset of cancer patients, severely impairing quality of life and diminishing response to therapies. Unlike starvation, cachexia is refractory to nutritional support and is driven by aberrant metabolic and inflammatory signals. Historically, the molecular underpinnings of this syndrome have remained elusive, particularly within distinct genetic subtypes of cancer such as STK11/LKB1-mutated NSCLC, which constitutes a clinically aggressive form with poor prognosis. The current study elucidates the direct contribution of tumor-secreted factors to systemic metabolic derailment.
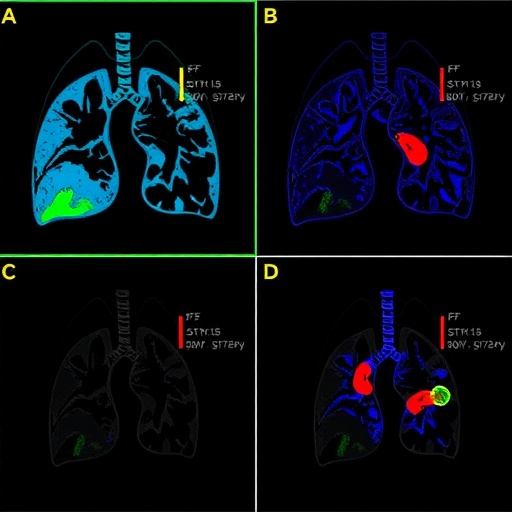
The researchers embarked on an integrative approach combining cutting-edge genomic profiling, in vivo modeling, and mechanistic cell biology to dissect the origins of cachexia in STK11/LKB1-mutated tumors. They identified GDF15 as a prominent secretory protein highly expressed by the tumor cells harboring these mutations. GDF15, a distant member of the transforming growth factor-beta (TGF-β) superfamily, has long been implicated in various stress responses but its role in cancer-associated weight loss was not fully understood. By delineating the tumor-autonomous upregulation of GDF15, the authors convincingly linked this factor to systemic metabolic dysregulation.
Using genetically engineered mouse models, the study demonstrated that elevated circulating GDF15 levels were sufficient to recapitulate the hallmark features of cachexia, including profound anorexia, muscle atrophy, and adipose tissue depletion. Critically, neutralization of GDF15 with specific antibodies ameliorated these symptoms, restoring muscle mass and improving overall survival. This provides compelling evidence that GDF15 is not merely a biomarker but an active mediator of the cachexia syndrome induced by STK11/LKB1-mutated NSCLC.
At a cellular signaling level, the study revealed that tumor-secreted GDF15 acts through a newly characterized receptor complex involving GDNF family receptor alpha-like (GFRAL) expressed in the hindbrain, specifically within regions controlling appetite and energy homeostasis. Binding of GDF15 to GFRAL initiates downstream signaling cascades that reduce food intake and enhance catabolic pathways, driving cachectic changes. This elegantly uncovers how a tumor-derived endocrine signal hijacks central nervous system circuits to wreak havoc on host metabolism.
The implications of this discovery are profound. By pinpointing GDF15 as a critical effector, the findings pivot the paradigm from viewing cachexia as a nonspecific inflammatory consequence to a tumor-directed endocrine phenomenon that can be therapeutically intercepted. This redefines the cachexia landscape and underscores the necessity of stratifying patients based on tumor genotype and secretory profiles when designing anti-cachexia interventions.
Furthermore, the study sheds light on why patients with STK11/LKB1 mutations frequently experience more severe cachexia and poorer clinical outcomes. The intrinsic genetic alterations within the tumor not only drive oncogenic growth but also instigate systemic metabolic disturbances through GDF15 secretion, creating a feed-forward loop of tumor progression and host debilitation. Thus, the tumor’s genotype influences disease biology at multiple levels.
Of particular note is the therapeutic potential illuminated by this research. Targeting GDF15 or its receptor GFRAL with monoclonal antibodies or small molecule inhibitors could offer a novel treatment avenue to mitigate cachexia, thereby improving patient stamina and responsiveness to conventional therapies such as chemotherapy and immunotherapy. The preclinical proof-of-concept studies in murine models provide a clear rationale for advancing such agents into clinical trials.
The research also calls attention to the diagnostic possibilities inherent in measuring circulating GDF15 as a predictive biomarker. Given its robust elevation in STK11/LKB1-mutated NSCLC-associated cachexia, GDF15 levels could guide oncologists in early identification of patients at risk for rapid wasting and tailor supportive care accordingly. This personalized medicine approach aligns with the broader goal of precision oncology.
From a mechanistic standpoint, the work encourages a reexamination of other tumor-derived factors that may contribute distinctively to cachexia in different cancer types or subtypes. It posits that cachexia is not a uniform syndrome but rather a constellation of tumor-genotype-specific endocrine effects that converge on host metabolism. Future research inspired by this model might unravel analogous pathways in other malignancies.
The study’s integration of multidisciplinary methodologies—ranging from transcriptomic analysis, proteomics, neurobiology, and mouse genetics—exemplifies the power of comprehensive investigation in confronting complex biological phenomena. Such rigor ensures that the findings are not only robust but also translatable, paving the way from bench to bedside with greater confidence.
Importantly, the findings stress the interplay between cancer pathophysiology and systemic host factors, emphasizing that effective cancer care requires addressing both tumor eradication and the maintenance of patient physiological reserves. Cachexia has long been an overlooked contributor to mortality, and this insight champions its inclusion as a therapeutic target within standard oncologic care.
This breakthrough also prompts broader questions regarding the impact of tumor-secreted factors on wider endocrine and metabolic systems. It opens avenues to explore whether similar mechanisms underlie other paraneoplastic syndromes and how they might be exploited therapeutically. The systemic ripple effects of tumor biology remain an exciting frontier in cancer research.
In light of these discoveries, oncologists and researchers should consider incorporating cachexia management strategies as a core component of treatment regimens, particularly for patients harboring STK11/LKB1 mutations. Clinical trials that evaluate GDF15-targeted therapies in combination with existing modalities could herald a new era where cancer-associated wasting is no longer an inexorable consequence of disease progression.
Moreover, the study enriches the conceptual framework through which we understand cancer’s systemic impact. By mechanistically connecting genomics with metabolism and neurobiology, it fosters a multidisciplinary dialogue that could revolutionize how we approach complex cancer syndromes beyond the tumor microenvironment.
In summary, the identification of tumor-secreted GDF15 as the linchpin in cancer cachexia associated with STK11/LKB1-mutated NSCLC marks a landmark achievement in oncology research. It exemplifies how elucidating tumor-host communication pathways can translate into tangible therapeutic targets, ultimately aiming to enhance survival and quality of life for lung cancer patients. As this field evolves, the integration of such mechanistic insights into clinical practice will be indispensable in overcoming the multifactorial challenges posed by cancer.
Subject of Research: Cancer cachexia mechanisms in STK11/LKB1-mutated non-small cell lung cancer mediated by tumor-secreted GDF15.
Article Title: Cancer cachexia in STK11/LKB1-mutated non-small cell lung cancer is dependent on tumor-secreted GDF15.
Article References:
Yu, J., Guo, T., Gupta, A. et al. Cancer cachexia in STK11/LKB1-mutated non-small cell lung cancer is dependent on tumor-secreted GDF15. Nat Commun (2026). https://doi.org/10.1038/s41467-026-68702-y
Image Credits: AI Generated
Tags: cancer cachexiaGDF15 role in cancergenomic profiling in cancer researchinflammatory signals in cachexiamechanisms of cancer-induced weight lossmetabolic syndrome in cancermuscle loss in cancer patientsnon-small cell lung cancerSTK11 mutant lung cancertargeted therapies for cachexiatherapeutic interventions for cancertumor-host interactions