Credit: © International Osteoporosis Foundation
Increased risk of fracture has been shown to be one of the complications arising from longstanding diabetes. With the worldwide increase in Type 2 Diabetes (T2D), in part due to aging populations, there is also increasing concern about how to identify and manage patients with diabetes who are at high risk of osteoporotic fracture.
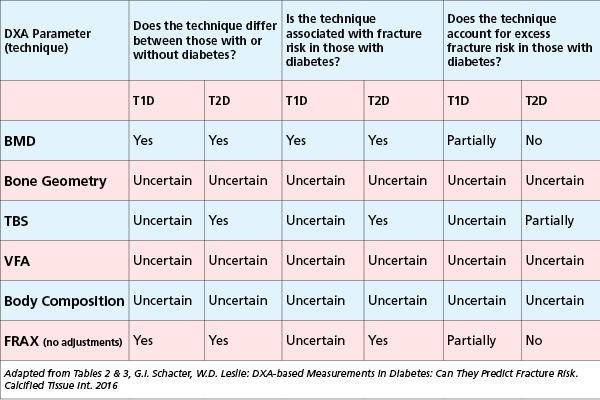
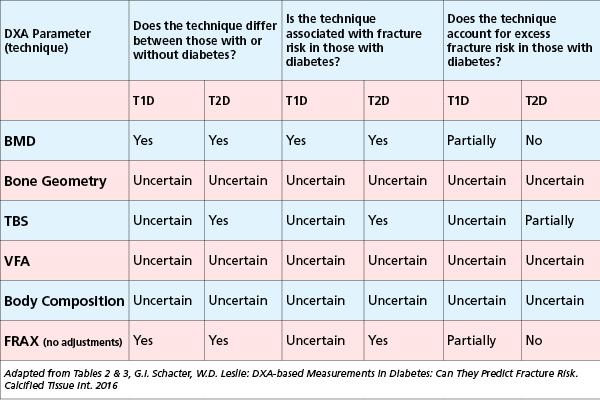
Osteoporosis is usually diagnosed from bone mineral density (BMD) measured by dual-energy X-ray absorptiometry (DXA). The authors reviewed data on skeletal parameters and techniques readily available from DXA scanning, and considered their utility in routine clinical practice for predicting fracture risk. DXA measures BMD as well these other applications and measurements: trabecular bone score (TBS), skeletal geometry and DXA-based finite-element analysis, vertebral fracture assessment (VFA), and body composition.
They also looked at fracture prediction tools, and specifically at the widely used Fracture Risk Assessment Tool (FRAX®) which is incorporated into modern DXA scanners. FRAX underestimates fracture risk in individuals with T2D – with factors contributing to this underestimation including the higher BMD observed in T2D, the greater risk for falls, and alterations in material strength. Nevertheless, several methods have been proposed to improve the performance FRAX in T2D.
The review summarizes the evidence for the effect of various DXA-derived skeletal parameters in T1D and T2D. In regard to whether they can be used to account for the excess fracture risk, the review concludes:
- In Type 1 Diabetes (T1D), BMD and FRAX (when secondary osteoporosis is included without BMD) only partially account for the excess risk of fracture in T1D. It is uncertain whether bone geometry, TBS, VFA or body composition account for excess fracture risk in T1D.
- In Type 2 Diabetes (T2D), BMD and FRAX can be used to stratify fracture risk, but do not account for the increased risk of fracture. However, several adjustments to the FRAX score can be made as proxies for T2D to inform the use of FRAX by primary care practitioners. Examples include the rheumatoid arthritis input (as a proxy for T2D), lumbar spine TBS (to adjust FRAX probability) or an altered hip T-score (lowered by 0.5 units). TBS is associated with increased fracture risk, and may partially account for excess risk of fracture. It remains uncertain whether bone geometry, VFA, or body composition differ between those with or without T2D, or whether they are associated with increased or excess fracture risk.
Lead author Professor William D. Leslie of the Department of Medicine, University of Manitoba, Canada stated:
"Diabetes is associated with increased fracture risk that is only partially reflected by the BMD reductions see in in T1D, and is underestimated in T2D where BMD is increased. While BMD from DXA still stratifies fracture risk in those with diabetes, additional measures that can be obtained from DXA help to identify high-risk patients. Incorporating this additional information into risk prediction models may help to avoid systematically underestimating the risk of osteoporosis-related fractures in people with diabetes."
###
Reference: Schacter G I, Leslie W D. DXA-Based Measurements in Diabetes: Can They Predict Fracture Risk? Calcif Tissue Int. DOI 10.1007/s00223-016-0191-x https://link.springer.com/article/10.1007/s00223-016-0191-x
Calcified Tissue International & Musculoskeletal Research
Calcified Tissue International & Musculoskeletal Research is a peer-reviewed journal which publishes original preclinical, translational and clinical research, and reviews concerning the structure and function of bone, and other musculoskeletal tissues in living organisms, as well as clinical studies of musculoskeletal disease. It includes studies of cell biology, molecular biology, intracellular signalling, and physiology, as well as research into the hormones, cytokines and other mediators that influence the musculoskeletal system. The journal also publishes clinical studies of relevance to bone disease, mineral metabolism, muscle function, and musculoskeletal interactions.
Editors in Chief: Stuart Ralston and René Rizzoli; Musculoskeletal Research Section Editor: Roger Fielding. http://link.springer.com/journal/223
> Become an IOF Professional member to freely access IOF scientific journals via the IOF website: https://www.iofbonehealth.org/become-member
About IOF
The International Osteoporosis Foundation (IOF) is the world's largest nongovernmental organization dedicated to the prevention, diagnosis and treatment of osteoporosis and related musculoskeletal diseases. IOF members, including committees of scientific researchers as well as 234 patient, medical and research societies in 99 locations, work together to make fracture prevention and healthy mobility a worldwide heath care priority. http://www.iofbonehealth.org / http://www.facebook.com/iofbonehealth @iofbonehealth
Media Contact
L. Misteli
[email protected]
41-229-940-100
@iofbonehealth
http://www.iofbonehealth.org