A groundbreaking breakthrough in neonatal respiratory monitoring has emerged from recent research employing Gas in Scattering Media Absorption Spectroscopy (GASMAS) to detect lung gas volumes on a breath-by-breath basis. This innovative study, published in Pediatric Research, introduces a cutting-edge technology capable of providing real-time insights into pulmonary function in neonates, potentially revolutionizing critical care in newborn medicine. Utilizing a high-fidelity neonatal mannequin, the research team led by Panaviene and colleagues has demonstrated the capacity of GASMAS to measure dynamic lung gas volumes non-invasively, heralding a significant advancement in both respiratory diagnostics and patient monitoring.
Lung function monitoring in neonates has long posed a considerable challenge due to the delicate and rapidly changing physiological parameters of newborns. Traditional methods, such as blood gas analysis or ventilator monitoring, offer limited temporal resolution and often involve invasive procedures that add risk and discomfort for these vulnerable patients. Against this backdrop, the adoption of GASMAS technology provides a novel optical approach that leverages the unique spectral signatures of gases trapped in biological tissues. By applying spectroscopic principles, GASMAS accurately quantifies gas concentrations—specifically those of molecular oxygen and water vapor—within the lung environment, enabling precise lung volume evaluation without direct contact or interference.
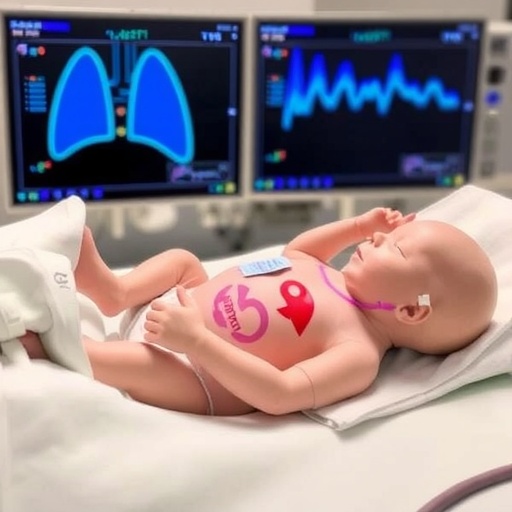
The neonatal mannequin used in this study serves as a crucial platform for simulating real-world clinical scenarios, allowing detailed calibration and validation of the GASMAS apparatus. This controlled environment affords researchers the ability to replicate varying respiratory patterns and lung conditions relevant to a broad spectrum of neonatal health states. By continuously measuring the lung volumes on a breath-by-breath basis, the investigators have shown consistent correlation between optical signals obtained via GASMAS and the known volumes programmed into the mechanical lung simulator of the mannequin. Such high-resolution data capture could significantly enhance clinicians’ ability to detect subtle changes in lung function that precede overt respiratory distress.
Technical implementation of GASMAS relies on near-infrared light passing through scattering tissues, with specific absorption peaks corresponding to the gaseous components within the lung’s alveolar spaces. By meticulously analyzing these modulated optical signals, the instrument deciphers the concentration levels and changes of pulmonary gases during the respiratory cycle. This spectroscopic technique offers remarkable temporal resolution, allowing for near-instantaneous feedback on lung volume fluctuations. Such capabilities open the door to not only tracking ventilation efficacy but also assessing the success of therapeutic interventions in real-time, a feat previously unattainable without invasive or cumbersome methods.
Beyond its clinical implications, the GASMAS technique’s non-invasive nature represents a pivotal step toward minimizing distress and potential harm in neonatal care. Conventional monitoring often includes procedures that can increase infection risk or require sedation, both of which are highly undesirable in fragile infants. The optical gas sensing method eliminates these concerns by forgoing physical intrusion, reducing the risk profile, and improving the comfort of neonatal patients. Additionally, the portability and speed of GASMAS technology may facilitate broader deployment across neonatal intensive care units (NICUs), offering standardized and reproducible lung volume monitoring that can enhance patient outcomes globally.
The study’s results have far-reaching implications for diagnosing and managing a host of neonatal pulmonary conditions, including respiratory distress syndrome, bronchopulmonary dysplasia, and apnea of prematurity. Early and precise detection of compromised lung function enables timely interventions, which are crucial in this delicate patient population. Moreover, continuous breath-by-breath monitoring supports tailored ventilator settings that adapt to the neonate’s immediate physiological status, reducing the risk of lung injury caused by over- or under-ventilation. This adaptability marks a significant leap toward personalized respiratory care in neonatology.
Importantly, the integration of GASMAS with existing respiratory support systems could pave the way for highly automated care environments, where sensor inputs continuously guide therapeutic decisions. Imagine a closed-loop ventilation system that adjusts parameters based on live spectroscopic feedback from the lungs, optimizing oxygen delivery while minimizing damage. Such systems could dramatically reduce the workload on healthcare providers, ensuring that neonates receive vigilant, real-time monitoring irrespective of nurse or physician availability, thus enhancing patient safety and care quality.
The research also touches upon the methodological challenges overcome to harness GASMAS in a scattering medium as complex as human lung tissue, albeit simulated here by a mannequin. Biological tissues scatter and absorb light in intricate ways that complicate spectroscopic measurements, but advances in optical modeling and calibration algorithms have allowed the team to isolate gas-specific signals reliably. This achievement not only demonstrates the technical feasibility of GASMAS for pulmonary monitoring but also lays the groundwork for future in vivo studies to verify and refine this approach in clinical settings.
Further exploration is warranted to extend this technology beyond mannequins and into live neonatal patients, where variables such as spontaneous movement, varying tissue properties, and heterogeneous lung pathology could influence signal acquisition. The refinement of sensor design, signal processing techniques, and adaptive calibration protocols will be critical to translating this promising approach into practical bedside tools that can withstand the complexities of real-world neonatal care scenarios.
Moreover, the potential applications of GASMAS extend beyond neonatology. Similar principles could be adapted for respiratory monitoring in pediatric and adult patients, especially those requiring prolonged mechanical ventilation or suffering from chronic pulmonary diseases. The non-invasive, continuous nature of the measurements confers broad utility, initiating a paradigm shift toward more precise and less distressing pulmonary diagnostics across age groups and clinical settings.
In a broader biomedical optics context, this research epitomizes the fusion of photonics, spectroscopy, and clinical medicine to solve pressing healthcare challenges. As biomedical optics technology continues to mature, integration with artificial intelligence for data interpretation and predictive analytics could further enhance the granularity and clinical value of GASMAS-derived parameters. Such integration would empower healthcare teams with sophisticated decision-support tools, enabling earlier identification of subtle pathophysiological changes and preemptive clinical actions.
The study by Panaviene and colleagues represents a landmark in respiratory physiology research, demonstrating the first breath-by-breath lung gas volume detection with GASMAS in a neonatal mannequin. This milestone embodies a synthesis of innovative optical physics, biomedical engineering, and neonatal medicine, promising a future where continuous, fiercely accurate lung monitoring is seamlessly woven into neonatal care. It is an inspiring development that reflects the transformative potential of multi-disciplinary research aimed at saving the most vulnerable lives—those of newborn infants.
As this field advances, the collaborative efforts among physicists, engineers, neonatologists, and clinical researchers will be essential to accelerate translation, optimize protocols, and ensure safety and efficacy in human subjects. The promise of GASMAS lies not only in its impressive technical achievements but also in its humanitarian potential to enhance neonatal survival and quality of life through more responsive and compassionate care.
In conclusion, breath-by-breath lung gas volume detection using GASMAS technology signifies a visionary leap forward in neonatology and pulmonary medicine. By marrying sophisticated spectroscopic instrumentation with the clinical imperative for non-invasive, precise monitoring, this research has set the stage for a new era of neonatal respiratory management. Continued innovation and clinical validation will determine how rapidly this promising technology transitions from mannequin models to routine use in NICUs worldwide, potentially reshaping neonatal care for generations to come.
Subject of Research: Breath-by-breath lung gas volume detection in neonates using Gas in Scattering Media Absorption Spectroscopy (GASMAS)
Article Title: Breath-by-breath lung gas volume detection using GASMAS in a neonatal mannequin
Article References:
Panaviene, J., Lanka, P., Grygoryev, K. et al. Breath-by-breath lung gas volume detection using GASMAS in a neonatal mannequin. Pediatr Res (2026). https://doi.org/10.1038/s41390-025-04699-2
Image Credits: AI Generated
DOI: 10 January 2026
Tags: advancements in newborn critical carebreath-by-breath lung gas detectionGASMAS technology in medicinehigh-fidelity neonatal mannequininnovative neonatal care solutionslung gas volume measurement techniquesneonatal patient monitoring innovationsneonatal respiratory monitoringnon-invasive lung function assessmentoptical gas detection methodspediatric respiratory diagnosticsreal-time pulmonary function monitoring