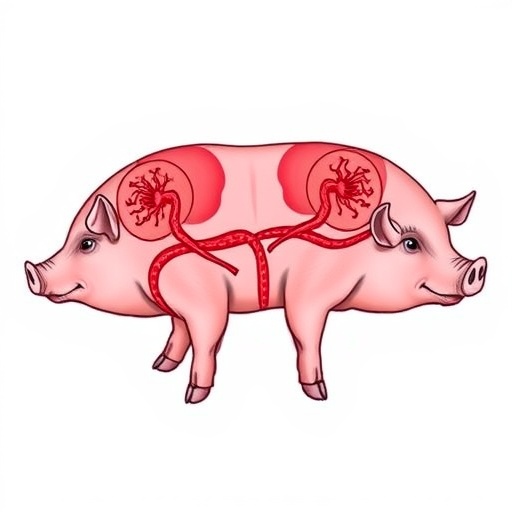
A groundbreaking advancement in regenerative medicine has been achieved by researchers at the Institute for Bioengineering of Catalonia (IBEC), in partnership with the Biomedical Research Institute of A Coruña (INIBIC) and numerous international collaborators. Their innovative approach enables the scalable production of human kidney organoids that can be integrated with porcine kidneys using ex vivo machine perfusion technology. This pioneering technique marks a significant milestone, bringing the promise of kidney organoid transplantation closer to clinical reality and opening new frontiers for personalized and regenerative therapies.
Human kidney organoids, miniature three-dimensional structures derived from pluripotent stem cells, mimic many key elements of kidney architecture and function, though they do not constitute fully developed organs. These organoids serve as invaluable models for understanding kidney development, enabling drug screening, disease modeling, and potentially providing a cellular therapy option to regenerate or repair damaged renal tissue. The primary challenge that has limited clinical translation until now has been the difficulty of generating kidney organoids in a scalable, consistent, and economically feasible manner.
The research team, led by Dr. Núria Montserrat, who has transitioned into her role as Catalonia’s Minister of Research and Universities, has developed a robust, systematic protocol that achieves mass production of thousands of kidney organoids using advanced microaggregation techniques combined with precise genetic engineering tools. This method allows for highly uniform organoid generation in a controlled laboratory environment within a significantly shortened timeframe, bypassing the requirement for complex reagents or components that typically inflate research costs.
One of the most innovative aspects of this study lies in the integration of human kidney organoids into living porcine kidneys maintained on normothermic machine perfusion devices. These organ support machines, commonly used in clinical transplantation, preserve organs ex vivo by delivering oxygenated blood at physiological temperatures, thereby enabling real-time organ function monitoring. By harnessing this technology, the team successfully implanted the organoids into the pig kidneys and observed their survival, integration, and functional stability over 24 to 48 hours both ex vivo and in vivo within the same animal model.
Machine perfusion permits continuous assessment of physiological parameters, such as renal filtration and tissue oxygenation, offering unprecedented insight into the viability and potential immune rejection of the implanted organoids. Remarkably, the human cells remained viable and engrafted without eliciting notable immune responses or signs of cytotoxicity. The transplanted porcine kidneys maintained functional integrity, highlighting the potential compatibility of cross-species organoid transplantation under controlled conditions.
This breakthrough approach outlines a visionary pathway toward organ regeneration prior to transplantation, wherein donor kidneys could be preconditioned and treated with human stem-cell-derived organoids to repair or enhance function before surgical implantation. Such capability could substantially improve transplant outcomes, reduce waiting times for transplant candidates, and alleviate the chronic shortage of viable donor organs. The translational nature of this work was bolstered by close collaboration with key clinical and research institutions, including Spain’s National Transplant Organisation and multiple biomedical research centers.
The methodological innovation hinges on the capability to produce large quantities of standardized organoids, overcoming one of the most significant bottlenecks in regenerative nephrology. By utilizing microaggregation and genetic editing platforms, the researchers optimized differentiation processes to yield reproducible kidney-specific cell types within the organoids, including renal tubules and podocytes—essential components for normal kidney function. Immunofluorescence imaging confirmed the spatial organization of these cells, demonstrating clear markers such as LTL, WT1, PODXL, and DAPI indicative of the organoids’ sophisticated cellular architecture.
Such high-throughput organoid generation coupled with real-time evaluation during ex vivo perfusion represents a quantum leap in tissue engineering. It unlocks the potential for precision medicine applications where individual patient-derived cells could be expanded and tested rapidly, facilitating personalized drug screening regimes or therapeutic interventions tailored to specific nephropathies or renal failure conditions. The scalability and efficiency of this system set a new benchmark for laboratory-to-clinic translation in bioengineering.
In addition to its biomedical implications, the study also emphasizes the critical role of interdisciplinary collaboration. Teams spanning bioengineering, transplant surgery, immunology, and stem cell biology from institutions across Europe and the United States jointly contributed to this research, highlighting a truly global effort to tackle complex challenges in organ regeneration. The involvement of medical technology companies specializing in organ perfusion devices underlines the alliance between academic research and industry innovation.
Looking forward, the research group aims to extend the window of organoid survival post-transplantation and explore the potential for full functional maturation within xenogeneic settings, ultimately aiming for clinical trials in human patients. Further research into immune modulation and vascular integration will be essential to achieve long-term stability and functionality of transformed organs. The promise of combining ex vivo regenerative techniques with advanced machine perfusion may redefine transplant medicine paradigms.
This groundbreaking publication, entitled “Systematic production of human kidney organoids for transplantation in porcine kidneys during ex vivo machine perfusion,” was recently featured in Nature Biomedical Engineering. It underscores a decade-long scientific journey driven by relentless pursuit of innovation to make regenerative therapies a clinical reality, highlighting how state-of-the-art bioengineering can synergize with clinical transplantation to save lives. The study’s interdisciplinary nature, scalability, and translational potential mark it as a seminal contribution poised to generate significant impact in medicine and organ bioengineering worldwide.
The Institute for Bioengineering of Catalonia, a leading center recognized for excellence in multidisciplinary bioengineering and life sciences research, continues to break ground in the field of organoid technology and tissue engineering. Their work exemplifies how strategic collaboration between universities, governmental agencies, and industry partners can accelerate revolutionary innovations, bridging the gap from bench to bedside in a socially impactful manner.
Subject of Research: Animals
Article Title: Systematic production of human kidney organoids for transplantation in porcine kidneys during ex vivo machine perfusion
News Publication Date: 31-Oct-2025
Web References: https://www.nature.com/articles/s41551-025-01542-1
References: Elena Garreta et al., Nature Biomedical Engineering (2025), DOI: 10.1038/s41551-025-01542-1
Image Credits: Institute for Bioengineering of Catalonia
Keywords: Organoids, Stem cells, CRISPRs, Medical technology, Regenerative medicine, Tissue engineering, Biomedical engineering, Nephropathies, Renal failure, Kidney
Tags: cellular therapy for renal tissueclinical translation of regenerative therapiesex vivo machine perfusion technologyhuman kidney organoids developmentinnovative transplantation techniqueskidney disease modeling researchorganoid integration with porcine kidneyspersonalized kidney therapiespluripotent stem cells applicationsregenerative medicine advancementsscalable organoid production methodstransplantation of pig kidneys