Postural Control in Children with Spastic Cerebral Palsy: Unveiling the Brain Lesion Connection
In the complex landscape of pediatric neurodevelopmental disorders, spastic cerebral palsy (sCP) holds particular significance due to its profound impact on motor function and quality of life. One of the most challenging aspects for children affected by sCP is maintaining postural control, which is crucial for everyday activities such as sitting, standing, and walking. Despite advances in clinical assessment and therapeutic interventions, the underlying causes of inter-individual variability in postural control within the spastic CP population remain a mystery. Traditional metrics, including CP topography and functional level classifications, have provided only limited explanatory power. However, a groundbreaking study published in Pediatric Research by Jacobs, Fiori, Guzzetta, and colleagues proposes that characteristics of brain lesions may serve as critical determinants of postural ability, opening new avenues for tailored rehabilitation.
The study addresses a pivotal gap in our understanding of spastic cerebral palsy. While previous research has extensively documented how brain lesions influence upper limb motor functions, little attention has been paid to their role in postural control. The authors hypothesized that the nature, location, and extent of brain lesions could be mechanistically linked to differences in postural stability observed among children with sCP. Using state-of-the-art neuroimaging techniques coupled with comprehensive postural assessments, the team examined these correlations with unprecedented precision. Their results not only highlight the heterogeneity of brain damage in sCP but also underline the indispensability of lesion characterization in predicting motor outcomes beyond arm functionality.
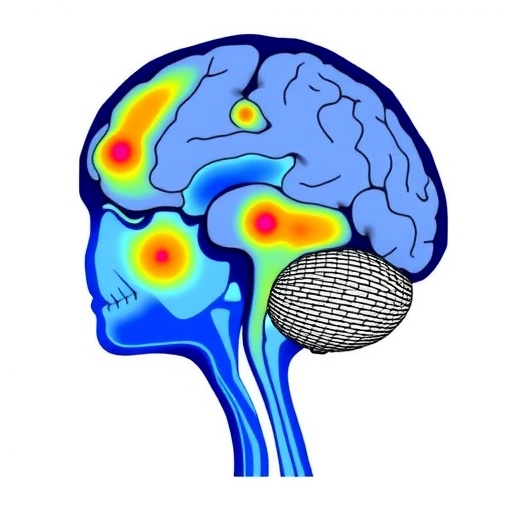
Postural control involves a complex interplay of sensory inputs, central processing, and musculoskeletal responses. It requires the integration of vestibular, somatosensory, and visual systems to maintain balance and orientation against gravitational forces. In children with spastic cerebral palsy, damage to brain areas mediating these sensory and motor processes might compromise this integrative capacity. The study systematically analyzed lesion patterns, including periventricular leukomalacia, cortical and subcortical injuries, and their spatial distribution relative to motor and sensory cortical regions. Intriguingly, specific lesion topographies were found to correspond with distinct postural control profiles, suggesting personalized neural substrates for balance impairments.
Beyond neuroanatomical insights, this research brings to light sophisticated neurophysiological mechanisms implicated in posture regulation. Lesions affecting the corticospinal tracts and secondary motor pathways were associated with diminished reflex modulation and impaired anticipatory postural adjustments. Moreover, damage to parietal regions—the hubs for sensory integration and spatial awareness—correlated strongly with increased postural sway and instability. These findings implicate disrupted sensorimotor integration as a driver of postural deficits. Such mechanistic understanding is paramount for developing targeted therapies that transcend conventional physical rehabilitation, potentially incorporating neuromodulation or brain-computer interface technologies to restore postural function.
The study’s methodology combined quantitative posturography with advanced magnetic resonance imaging (MRI) to juxtapose functional impairments against brain morphology and lesion characteristics. Participants’ postural stability was measured during static and dynamic tasks, and lesion mapping included volumetric analyses and diffusion tensor imaging (DTI) to assess white matter integrity. This multimodal approach allowed the researchers to construct detailed brain-behavior models, revealing nuanced relationships previously obscured by more generalized assessments. Importantly, the study recognized and controlled for confounding factors such as the Gross Motor Function Classification System (GMFCS) levels, underscoring the independent predictive value of lesion topology for postural control outcomes.
One of the most compelling implications of this research concerns clinical prognostic models for children with sCP. Current assessment tools often rely upon visible motor impairments and functional classification, which provide limited foresight into the trajectory of postural control development. By integrating brain lesion characterization, clinicians could better predict which children are at higher risk for severe balance impairments and tailor early intervention strategies accordingly. This stratification approach could revolutionize rehabilitation planning, optimizing resource allocation and maximizing functional gains during critical periods of neuroplasticity in childhood.
Additionally, the study advocates for a paradigm shift in therapeutic design. Traditional approaches focusing only on motor training might benefit from incorporating sensory integration therapies aimed at enhancing compensatory pathways. The link between specific lesion sites and sensorimotor deficits highlights potential targets for novel treatment modalities including virtual reality (VR)-based balance training, robotic-assisted therapy, and neuromodulatory interventions such as transcranial magnetic stimulation (TMS). Personalized rehabilitation informed by precise lesion mapping might improve not only postural control but also the overall functional independence and quality of life for these children.
Moreover, the researchers emphasize the importance of longitudinal studies to capture the dynamic evolution of postural control and brain reorganization after injury. Neuroplastic changes over time may reshape the influence of lesions on motor function, suggesting that early identification and intervention could capitalize on adaptive neural mechanisms. Future research endeavors might focus on tracking neurodevelopmental trajectories in relation to lesion characteristics to understand critical windows for intervention and to predict long-term functional outcomes more accurately.
From a broader neurodevelopmental perspective, this research enriches our understanding of how focal brain injuries manifest as complex motor phenotypes. Cerebral palsy, traditionally viewed through a motor impairment lens, can now be reconsidered as a disorder with distinct neuroanatomical fingerprints that influence multiple domains of sensorimotor integration. This insight aligns with emerging neuroscience frameworks that prioritize brain network connectivity and functional organization over simplistic lesion localization, reaffirming the heterogeneity and plasticity inherent in neurodevelopmental conditions.
Furthermore, this study challenges the classical view that topographical classifications of cerebral palsy (hemiplegia, diplegia, quadriplegia) sufficiently explain functional limitations. By underscoring the predictive role of detailed lesion characteristics, the authors prompt a more nuanced approach to subclassifying sCP patients. This could spur refinement in diagnostic criteria and foster precision medicine approaches, where interventions are tailored not by gross motor patterns alone but by underlying neurobiological substrates. Such a paradigm has profound implications for enhancing therapeutic efficacy and patient outcomes in pediatric neurorehabilitation.
Technologically, the integration of advanced imaging modalities, computational lesion mapping, and quantitative motor assessments exemplifies the potential of interdisciplinary research. The combination of neuroimaging data with machine learning algorithms might in the future enable automated predictions of postural control based on lesion profiles. This synergy between neuroscience, engineering, and clinical practice heralds a new era where data-driven approaches can meaningfully transform care pathways for children with cerebral palsy and other neurodevelopmental disorders.
In conclusion, the study by Jacobs and colleagues marks a pivotal advance in cerebral palsy research, providing compelling evidence that brain lesion characteristics substantially influence postural control in children with spastic CP. By bridging neuroanatomical, physiological, and functional domains, this research opens exciting prospects for precision diagnostics, individualized rehabilitation, and ultimately enhanced quality of life for affected children. As researchers and clinicians integrate these insights into practice, the future holds great promise for unlocking the full potential of neuroplasticity and restoring motor function in pediatric populations challenged by brain injury.
Subject of Research: Postural control in children with spastic cerebral palsy related to brain lesion characteristics
Article Title: Postural control in children with spastic cerebral palsy: the role of brain lesion characteristics
Article References:
Jacobs, N., Fiori, S., Guzzetta, A. et al. Postural control in children with spastic cerebral palsy: the role of brain lesion characteristics. Pediatr Res (2026). https://doi.org/10.1038/s41390-025-04741-3
Image Credits: AI Generated
DOI: 13 January 2026
Tags: brain lesions and motor functioncharacteristics of brain lesions in childrenfunctional level classifications in cerebral palsyimpact of brain lesions on postureinter-individual variability in CPpediatric neurodevelopmental disordersPediatric Research on cerebral palsypostural control in spastic cerebral palsyrehabilitation strategies for spastic CPsitting standing walking challenges in CPtailored interventions for spastic CPunderstanding postural stability in CP