In a remarkable leap forward for oncology and regenerative medicine, a recent study reveals a pioneering approach to treating tumorous bone defects by harnessing the power of borosilicate bioactive glass combined with moderate magnetic hyperthermia. This multifaceted strategy uniquely addresses the dual challenge of eradicating malignant cells while simultaneously promoting bone regeneration — an intricate balance that has eluded researchers for decades. The innovative approach, published in Nature Communications, offers a beacon of hope for patients suffering from bone cancers and related complications, signaling a potential paradigm shift in clinical therapeutics.
Bone tumors present an arduous clinical challenge, not only due to their destructive effects on skeletal integrity but also because traditional treatments often impair the natural regenerative processes. Chemotherapy and radiation, while effective at removing cancerous cells, frequently result in collateral damage to healthy bone tissue. Surgical excision commonly leads to significant bone defects, necessitating sophisticated reconstructive techniques that are complicated by the tumor microenvironment’s hostile conditions. The new approach devised by Fan, Liu, Zhang, and their colleagues strategically capitalizes on advanced materials science and bioengineering to overcome these hurdles.
The crux of this groundbreaking research is the employment of borosilicate bioactive glass, a composite material known for its osteoconductive and osteoinductive properties. Unlike conventional bioactive glasses, the borosilicate variant offers enhanced dissolution kinetics and ion release profiles, which are critical for stimulating cellular activities linked to bone growth. Its unique chemical composition allows it to interact dynamically with the biological milieu, facilitating the formation of hydroxycarbonate apatite layers that serve as a natural scaffold for bone cell attachment and proliferation.
What sets this novel methodology apart is the integration of moderate magnetic hyperthermia — a technique by which magnetic nanoparticles embedded within the bioactive glass matrix generate localized heat when subjected to an alternating magnetic field. This mild, controlled thermal stimulus selectively ablates tumor cells by exploiting their heightened sensitivity to temperature elevations, all while sparing surrounding healthy tissue. The synergy between the bioactive glass’s regenerative cues and hyperthermia’s tumoricidal effects represents a sophisticated therapeutic cocktail.
At the molecular level, the bioactive glass releases biologically relevant ions such as boron, silicon, and calcium, which play pivotal roles in activating signaling pathways responsible for osteoblast differentiation and angiogenesis. This ion-mediated stimulation ensures that, as hyperthermia reduces tumor burden, the damaged bone matrix is primed for rapid and effective rebuilding. Importantly, the moderate temperature range (typically between 41–45°C) used in this approach avoids the adverse effects of higher-temperature hyperthermia, such as necrosis of healthy tissues and inflammatory responses that could impede healing.
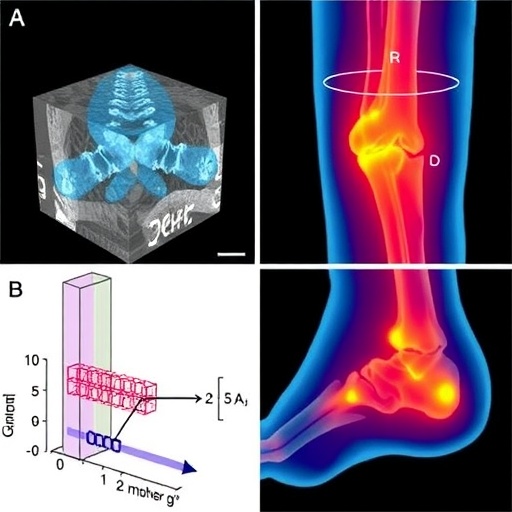
The experimental validation involved rigorous in vitro and in vivo assays, demonstrating the dual-function capability of the borosilicate bioactive glass scaffold. Cell viability assays confirmed preferential cytotoxicity against osteosarcoma cells under magnetic hyperthermia conditions, while assays involving mesenchymal stem cells illustrated enhanced proliferation and differentiation on the glass surface. Animal models showed promising results, with significant tumor decline accompanied by robust new bone formation within critical defect sites. These findings underscore the potential clinical applicability of the platform.
Moreover, the study delves deeply into the physicochemical characterization of the borosilicate glass material. Employing techniques such as scanning electron microscopy, X-ray diffraction, and Fourier-transform infrared spectroscopy, the researchers established the morphology, crystallinity, and chemical bonding attributes crucial for its function. These analyses validate that the optimized glass composition maintains structural integrity during hyperthermia and bioresorbs at a rate conducive to tissue remodeling without eliciting adverse reactions.
The innovation lies equally in the development of a magnetic field delivery system that permits fine-tuned control over the heating process. Using superparamagnetic nanoparticles embedded homogeneously in the borosilicate matrix, the researchers achieved consistent temperature elevation throughout the implant site. This precision circumvents the typical limitations of magnetic hyperthermia where uneven heating can cause ineffective tumor ablation or damage to healthy structures. Consequently, the treatment can be administered repeatedly as needed during longitudinal care.
An additional noteworthy aspect of this strategy is its compatibility with minimally invasive surgical procedures. The bioactive glass scaffold can be molded into custom shapes corresponding to patient-specific bone defects, a property that facilitates its use in complex anatomical locations often affected by tumors. This personalized approach aligns with the broader trend in medicine toward bespoke implants and therapeutics that maximize efficacy while reducing complications.
Beyond the immediate therapeutic implications, the study also sheds light on the immunological interplay engendered by the treatment. Preliminary investigations revealed that moderate hyperthermia delivered via the borosilicate glass scaffold modifies the tumor microenvironment by promoting immune cell infiltration and activation. This enhanced immunogenicity may synergize with emerging immunotherapies, suggesting avenues for combination treatments that harness the body’s immune defenses alongside physical tumor ablation and regeneration.
Importantly, the safety profile of this approach was rigorously assessed. Toxicological studies reported negligible systemic toxicity and minimal inflammatory responses after the bioactive glass implantation and repeated magnetic hyperthermia sessions. This contrasts favorably with more aggressive thermal tumor treatments, positioning the technique as a potentially safer alternative or adjunct to conventional therapies in orthopedic oncology.
From a translational perspective, the study’s authors highlight the scalability and manufacturability of the borosilicate bioactive glass composite. The materials and processing methods are compatible with current medical device fabrication standards, suggesting a pathway toward large-scale production and clinical deployment. Regulatory considerations will of course require extensive further testing; nevertheless, the foundational research lays a robust groundwork.
In conclusion, the innovative fusion of borosilicate bioactive glass with moderate magnetic hyperthermia represents a milestone in the fight against bone tumors. It skillfully addresses the long-standing problem of eradicating malignancy without sacrificing the delicate process of bone healing, bridging oncology and regenerative medicine in ways previously unattainable. As the scientific community continues to validate and refine this approach, it holds immense promise for revolutionizing treatment paradigms and improving patient outcomes in skeletal oncology.
The authors’ revelations epitomize the transformative potential residing at the intersection of materials science, bioengineering, and clinical medicine. They underscore the importance of multidisciplinary collaborations to tackle complex diseases with nuanced therapeutic strategies that transcend traditional single-modality interventions. This work undoubtedly inspires future research exploring combinatorial treatments that simultaneously target disease eradication and tissue regeneration.
As clinical trials progress and technological refinements emerge, the patient care landscape for those afflicted with bone tumors could be dramatically altered. The integration of smart biomaterials capable of responding to external stimuli like magnetic fields paves the way for next-generation implantable devices that do more than replace damaged structures — they actively contribute to the healing process while suppressing disease recurrence.
The broader implications for regenerative medicine are equally exciting. The principles demonstrated here could inform the development of similar therapeutic platforms tailored for soft tissue tumors, cartilage defects, or even neurodegenerative conditions where controlled hyperthermia and bioactive scaffolding could synergistically enhance repair while mitigating pathological processes.
In an era where personalization, precision, and biocompatibility define the frontier of therapeutic innovation, this pioneering research epitomizes the cutting edge. The borosilicate bioactive glass and moderate magnetic hyperthermia strategy not only confronts one of medicine’s most challenging dilemmas but also offers a versatile platform with vast potential applications — a true testament to the power of innovative science to transform lives.
Subject of Research: Tumorous bone regeneration using borosilicate bioactive glass combined with moderate magnetic hyperthermia for simultaneous tumor ablation and bone repair.
Article Title: A strategy for challenging tumorous bone regeneration by borosilicate bioactive glass boosting moderate magnetic hyperthermia.
Article References:
Fan, M., Liu, C., Zhang, Y. et al. A strategy for challenging tumorous bone regeneration by borosilicate bioactive glass boosting moderate magnetic hyperthermia. Nat Commun 16, 8057 (2025). https://doi.org/10.1038/s41467-025-63270-z
Image Credits: AI Generated
Tags: advanced materials in medicinebioactive glass for bone regenerationborosilicate glass in oncologyclinical applications of borosilicate glassdual approach to bone cancer therapyinnovative cancer treatment strategiesmagnetic hyperthermia for bone tumorsosteoconductive materials in oncologyovercoming bone tumor challengesparadigm shift in bone cancer therapeuticsregenerative medicine for bone defectstumor microenvironment and treatment