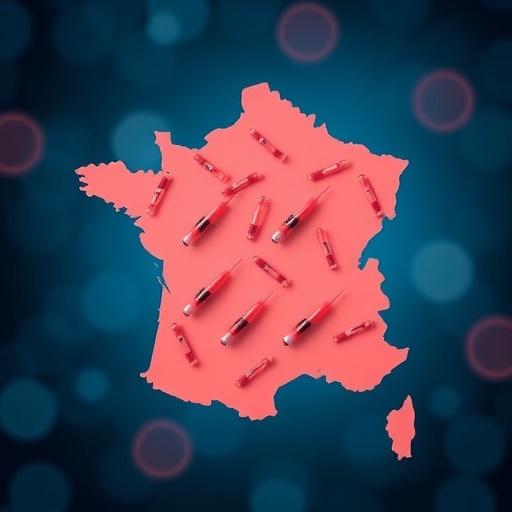
In recent years, the challenge of increasing human papillomavirus (HPV) vaccination coverage has become a critical public health objective, particularly in countries such as France, where vaccination rates lag behind those of other developed nations. A groundbreaking study led by Thilly, Michel, Bruel, and colleagues, recently published in Nature Communications, sheds light on the delicate balance required to boost HPV vaccine uptake effectively without inciting counterproductive backlash. Their research provides a crucial roadmap for policymakers, public health officials, and medical professionals aiming to optimize immunization strategies while navigating complex social and psychological landscapes.
Human papillomavirus remains one of the most common sexually transmitted infections globally, with certain high-risk strains directly implicated in the development of cervical cancer, as well as other anogenital and oropharyngeal malignancies. The advent of prophylactic HPV vaccines has dramatically transformed the potential for disease prevention, yet despite demonstrated safety and efficacy, vaccine coverage remains suboptimal in many regions. France, in particular, has faced notable obstacles, including vaccine hesitancy, misinformation, and logistical challenges, underscoring an urgent need for refined approaches.
The team’s study meticulously analyzes both historical and contemporary vaccination data, employing advanced epidemiological modeling to project the long-term impact of various intervention tactics. This comprehensive analysis identifies key drivers behind successful vaccine dissemination while cautioning against hasty policy implementations that risk eroding public trust. Notably, the authors emphasize the necessity of sustaining clear, transparent communication channels and engaging diverse community stakeholders to enhance acceptance rates.
.adsslot_NYjm2oEIpa{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_NYjm2oEIpa{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_NYjm2oEIpa{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
A notable dimension of the research involves dissecting the sociocultural context unique to France. The authors explore how historical skepticism towards vaccines, compounded by a complex healthcare infrastructure and variable access patterns, has contributed to a reluctance that cannot be overcome through aggressive mandates alone. Instead, the study advocates for calibrated, culturally sensitive engagement that addresses legitimate concerns without compromising urgency—a nuanced stance that challenges more conventional one-size-fits-all approaches.
Underpinning their recommendations is a rich corpus of immunological and virological insights. The study explicates the mechanism by which HPV vaccines generate robust humoral immunity, predominantly through stimulation of neutralizing antibodies targeting the viral L1 protein. By neutralizing the virus before cellular infection, these vaccines not only reduce individual risk but also contribute to herd immunity. This underpinning biological knowledge reinforces the strategic importance of achieving widespread coverage, particularly among adolescents prior to potential HPV exposure.
Moreover, the authors detail how vaccine efficacy varies depending on timing and adherence to the full dosing schedule. Real-world data highlights that partial immunization, while beneficial, falls short of providing optimal protection. This insight informs their advocacy for not only improving initial uptake but also ensuring regime completion, which they propose could be supported by innovative reminder systems and coordinated school-based programs.
Critically, the study also addresses the risks of overzealous or rushed vaccination campaigns, which might exacerbate vaccine hesitancy through perceived coercion or insufficient educational support. The researchers cite psychological theories related to risk perception and cognitive bias, arguing that rushed policies risk triggering reactance—a defensive response against perceived threats to personal autonomy. As such, the team recommends a phased approach, integrating feedback loops and continuous monitoring to adapt strategies dynamically.
Public health officials have historically faced significant challenges in balancing urgency against public sentiment, and this study serves as a timely reminder of this enduring tension. The research highlights examples from other high-income countries where carefully tailored communication campaigns, coupled with accessible vaccination services, yielded marked improvements in coverage and subsequent declines in HPV-related disease incidence.
Technological innovations also feature prominently in the authors’ proposed solutions. They explore the potential role of digital platforms and artificial intelligence in personalizing vaccine outreach and education, potentially mitigating misinformation and enhancing individualized engagement. Digital health tools could facilitate data-driven decision-making, optimizing resource allocation and enabling scalable, responsive interventions—a crucial advancement given the complexity of HPV vaccination dynamics.
Furthermore, the article delves into the economic implications of improved vaccination coverage. By preventing HPV-related cancers and the substantial healthcare costs associated with treatment, enhanced immunization programs represent not only a moral imperative but also a cost-effective public investment. Health economists within the team provide models demonstrating substantial long-term savings achievable through moderate but sustained increases in vaccine uptake.
The ethical dimensions of HPV vaccination policies are also thoughtfully examined. The authors contend that respecting patient autonomy must be balanced with public health imperatives, particularly when considering mandates for adolescents. They argue for policies that empower informed consent supported by community engagement rather than top-down enforcement, promoting trust and voluntary acceptance as pillars of a successful program.
Importantly, the research highlights the need for targeted efforts addressing disparities in vaccine access and acceptance. Marginalized populations—whether due to socioeconomic status, geographic location, or cultural factors—are often underserved by mainstream approaches. Tailored outreach combining linguistic, cultural, and logistical adaptations can bridge these gaps, ensuring equity in the benefits conferred by HPV vaccination.
The study’s collaborative approach, involving epidemiologists, immunologists, behavioral scientists, and policy analysts, exemplifies the interdisciplinary rigor necessary to tackle multifaceted public health challenges. By integrating diverse expertise, the team produces recommendations grounded in empirical evidence yet sensitive to real-world complexities.
Ultimately, this work underscores an urgent message distilled in the article’s title: there is a clear need to act decisively to improve HPV vaccination coverage in France, but such action must be measured, deliberate, and contextually nuanced. The consequences of missteps are significant, potentially reversing public gains and undermining confidence in vaccination programs more broadly.
As France and other nations grapple with how best to implement and scale HPV vaccination initiatives, this study offers a vital resource. It champions strategies that balance scientific rigor with empathetic public engagement, setting a paradigm for future efforts to prevent HPV-associated cancers worldwide. The lessons articulated herein resonate well beyond the French context, providing a blueprint for harnessing vaccination as a powerful tool in global cancer prevention.
Subject of Research: Strategies and considerations for improving human papillomavirus vaccination coverage in France, with an emphasis on balancing effective public health action and public acceptance.
Article Title: Improving human papillomavirus vaccination coverage in France: a need to act but not to rush.
Article References:
Thilly, N., Michel, M., Bruel, S. et al. Improving human papillomavirus vaccination coverage in France: a need to act but not to rush. Nat Commun 16, 5346 (2025). https://doi.org/10.1038/s41467-025-60874-3
Image Credits: AI Generated
Tags: addressing logistical challenges in vaccinationadvanced epidemiological modeling for vaccinationbalancing vaccine uptake and public perceptioncervical cancer prevention through vaccinationeffective public health interventionsHPV vaccination strategies in Francehuman papillomavirus infection preventionincreasing HPV vaccine coveragelong-term impact of HPV vaccination programsoptimizing immunization strategiespublic health objectives in Francevaccine hesitancy and misinformation